This week in our psychedelic news roundup, we delve deep into a series of groundbreaking discoveries and regulatory discussions making waves in the realm of psychedelic research and advocacy. The Special Ops veterans have found remarkable relief from PTSD through an innovative treatment in Mexico, igniting further interest in the therapeutic potential of psychedelics. Concurrently, a nasal spray formulation of Esketamine is showing promising results against treatment-resistant depression, challenging traditional approaches. The Eureka City Council, influenced by active proponents of legalization, is contemplating a resolution to prioritize the decriminalization of certain psychedelic substances. Up north, PsyCan’s latest white paper offers an in-depth examination of the current landscape of psychedelic usage in Canada, advocating for pivotal reforms to broaden patient access. Dive in as we explore these transformative developments in the rapidly evolving world of psychedelics.
Notable Psychedelic Studies This Week

A groundbreaking study is shifting the spotlight from the often debated high-dose treatments to the more subtle yet intriguing realm of ‘microdosing’.
Researchers involved with the study embarked on an innovative endeavor to formulate a credible microdosing regimen using rats. This regimen involved systematically administering psilocybin in doses tailored to its interaction with the rat brain’s 5-HT2A receptors.
The early results? In this enlightening exploration, the rats impressively weathered the recurring doses, showing no indications of mood disturbances, heightened anxiety, or shifts in their typical movement patterns. Furthermore, there weren’t any observable interruptions in their reflex responses nor any indications that the treatment caused the 5-HT2A receptors to become less responsive or receptive.
The rodent subjects demonstrate tolerance for the psychedelic compound and enhanced resilience to external stressors, accompanied by a marked reduction in compulsive behaviors. Notably, a significant increase in neural connectivity—particularly within the thalamus, a central region associated with decision-making—provides compelling insights.

Many special operations forces veterans often don’t find relief from conventional therapeutic methods. However, a recent analysis has revealed that a treatment involving two specific psychedelic substances was effective in alleviating symptoms of depression and anxiety, and it also enhanced cognitive abilities. These veterans underwent this unique treatment at a clinic in Mexico.
The therapeutic approach combined Ibogaine hydrochloride, which is extracted from the West African iboga plant, with 5-MeO-DMT, a psychedelic compound produced by the Colorado River toad. Both of these compounds are currently categorized as Schedule I drugs in the U.S.
Beyond reducing symptoms of PTSD, this treatment also addressed cognitive dysfunctions associated with traumatic brain injuries. This discovery was of significant interest to the research team from The Ohio State University that carried out the analysis.
In general, participants indicated significant enhancements in their PTSD symptoms, feelings of depression, anxiety levels, sleep quality, and anger management from the start of the treatment to a check-up one month later. These benefits persisted at the three- and six-month evaluations. Furthermore, there were sustained declines in impairment and post-traumatic symptoms for half a year, accompanied by considerable growth in adaptability and mental performance.
More details of the study can be found here.
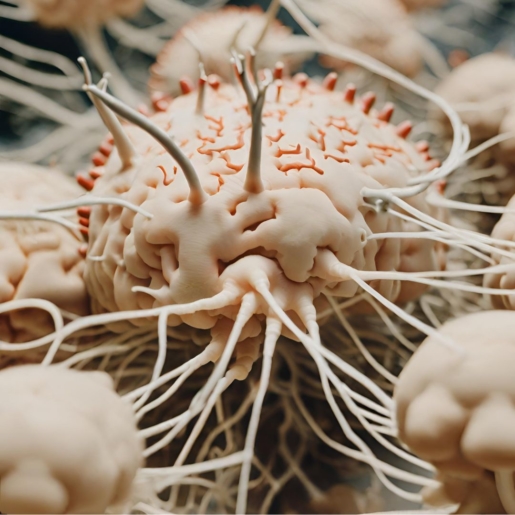
The human brain possesses the ability to adapt, but this often occurs slowly and demands significant effort. This plasticity is supported by scientific studies, suggesting that engaging in new activities can lead to detectable neural changes. Many people yearn for faster adaptability, especially when addressing personal challenges like mental health issues. While trauma can rapidly alter the brain, positive experiences can also induce swift, beneficial changes, highlighting the brain’s complex and responsive nature.
Psychedelic-assisted psychotherapy taps into a natural neural mechanism of accelerated change and transformations. How? By speeding up new connections between neurons in the brain via spine formations.
Historically, the belief was that persistent spine growth could only occur with concentrated, repeated cognitive effort. Yet, this week’s psychedelic news spotlights a study at Yale showed quick spine growth in the frontal cortex of mice after a single dose of psilocybin. The results indicated a roughly 10% rise in spine formation in mice exposed to this mushroom-derived compound. This growth was evident a day post-treatment and lasted for several weeks.

Microdosing advocates believe taking small amounts of certain psychedelic compounds can boost creativity, elevate mood, and sharpen focus, among other benefits. Yet, a study published this summer in the Journal of Psychopharmacology suggests that sustained microdosing might pose health risks. The researchers specifically highlighted concerns regarding a potential link between consistent microdosing and valvular heart disease (VHD).
Researchers have expressed concerns about the potential interaction between minute amounts of psychedelics and a specific bodily receptor called 5-HT2B. This receptor connects with the serotonin neurotransmitter and controls various body functions, including those related to the heart.
Beginning with the substance that poses the most significant potential danger: Psilocin, the active component of psilocybin, has a strong binding affinity to the 5-HT2B receptor, even more so than to its primary target receptor, 5-HT2A. This suggests that psilocin may carry a higher risk for VHD when used for microdosing than other psychedelics.
LSD, although exhibiting a balance in potency between its main target receptor, 5-HT2A and the 5-HT2B receptor, presents a potential danger for VHD. The body’s individual response to the substance, combined with varied dosing practices, might mean that there is only a sufficient safety buffer sometimes.
Due to its reduced potency, Mescaline leaves uncertainties about its effects on the 5-HT2B receptor. Nonetheless, when considering its binding strength and plasma concentration levels, there’s a hint of a narrow safety threshold, implying a possible risk.
While DMT shows a slim safety margin, its exceptionally brief duration in the system could mitigate some of the risks compared to the other compounds mentioned.
Interestingly, despite microdosing’s rising trend, there aren’t many reported VHD cases. Researchers, however, warn that this might be because the practice is relatively new, and few might have microdosed long enough for VHD symptoms to appear.

A nasal spray formulation of Esketamine showed greater efficacy in treating treatment-resistant depression compared to a widely recognized medication, according to a study released on Wednesday in The New England Journal of Medicine.
Esketamine is a stronger variant of ketamine, a long-standing anesthetic used in depression treatment. Janssen Pharmaceuticals markets this nasal spray as Spravato, which received the Food and Drug Administration’s approval for addressing treatment-resistant depression in 2019. The research, sponsored by Janssen, was conducted in 24 nations spanning Africa, Asia, Europe, and South America.
In the research, 336 adults with hard-to-treat depression were given nasal esketamine alongside their usual antidepressants, either an SSRI or an SNRI. In contrast, 340 participants were prescribed quetiapine, the generic form of the antipsychotic drug Seroquel, which has been available since 2007 and occasionally enhances the effectiveness of antidepressants in those with stubborn depression.
By the end of 8 weeks, 27.1% of those on Esketamine experienced significant symptom relief, as opposed to 17.6% in the quetiapine group. By week 32, of those who achieved symptom relief at 8 weeks, 21.7% on Esketamine sustained their improvement compared to 14.1% on quetiapine.
Notable Policy Moves This Week
Over the past weekend, there were modest changes to the policy concerning psychedelic drugs in California.
Governor Gavin Newsom ratified the legislation on Saturday. This move permits physicians in California to recommend psilocybin, MDMA, and other Schedule 1 prohibited substances to their patients, provided these drugs are reclassified under the federal Controlled Substances Act or given clearance by the federal Food and Drug Administration.
Get the details in our recent coverage here.

A team promoting the legalization of specific psychedelic plants and fungi has influenced the Eureka City Council to consider the topic in their upcoming session. Decriminalize Nature Humboldt members have been at several recent council events to get a resolution approved.
The proposal, if approved, would prioritize the enforcement related to possessing entheogens, including substances like ayahuasca and psilocybin mushrooms, as a low concern for the local police.
While the current proposal aims to give individuals the confidence to use these substances for mental health reasons without fearing legal repercussions, it also emphasizes that trading these substances would remain prohibited. The overarching goal is to support community-driven healing, especially considering the mental health challenges faced in Humboldt County.

PsyCan, a non-profit association that speaks for psychedelic medicinal and therapeutic businesses in Canada, has unveiled a recent white paper discussing psychedelics within the country, as reported on October 3rd, 2023. Spanning 99 pages, the document named “Beyond the Special Access Program—An Examination and Proposal on Psychedelic Usage in Canada” delves into the prevailing regulations in Canada and articulates its advocacy for changes that could broaden the reach of psychedelic treatments to more patients.
At present, the only legitimate channel for Canadians to obtain psychedelics is through the Special Access Program (SAP). This program facilitates patient access to psychedelic therapies for specific mental health issues, evaluated on an individual basis. However, the document’s authors highlight that such a system imposes excessive constraints on those looking for these treatments.
The suggested strategies are set to be implemented in both the near and distant future, encompassing:
- Swift enhancements to the operational standards of the Special Access Program, aiming for greater clarity and certainty while minimizing both the workload and wait time for those applying.
- Crafting a separate medical psychedelic accessibility initiative beyond the SAP, with the primary objective of quickly shielding patients from the drug conflict’s forefront.
- Creation of a National Psychedelic Access Committee, drawing inspiration from the National Cannabis Legalization Task Force. This group’s primary responsibility would be to organize extensive, area-specific, and multi-party discussions to explore varied pathways for both therapeutic and recreational psychedelic access.
One of the primary insights drawn mentions the evolving nature of psychedelic perceptions worldwide: “Given the mounting evidence regarding the safety and benefits of psychedelic treatments, there has been a notable shift in international regulations in recent times. This momentum suggests more transformations are on the horizon, emphasizing the importance of contemplating methods to enhance access to these therapies while ensuring adequate measures to mitigate potential risks and optimize the positive impacts of psychedelics on public well-being.”
