What You Should Know:
– The Centers for Medicare & Medicaid Services (CMS) has taken a bold step towards improving care for individuals with both mental health conditions and substance use disorders (SUD), announcing the “Innovation in Behavioral Health (IBH)” Model.
– This IBH model holds immense promise for transforming how we address the complex healthcare needs of individuals struggling with both mental and physical health challenges. By focusing on integrated care, addressing social determinants, and promoting health equity, the IBH Model has the potential to significantly improve the lives of millions of Americans.
Bridging the Gap: Addressing Dual Needs for Better Health Outcomes
Medicaid and Medicare populations experience disproportionately higher rates of mental health conditions and/or SUD, often leading to poor health outcomes and premature death. This can be attributed to fragmented healthcare systems, limited access to care, and underlying social issues.
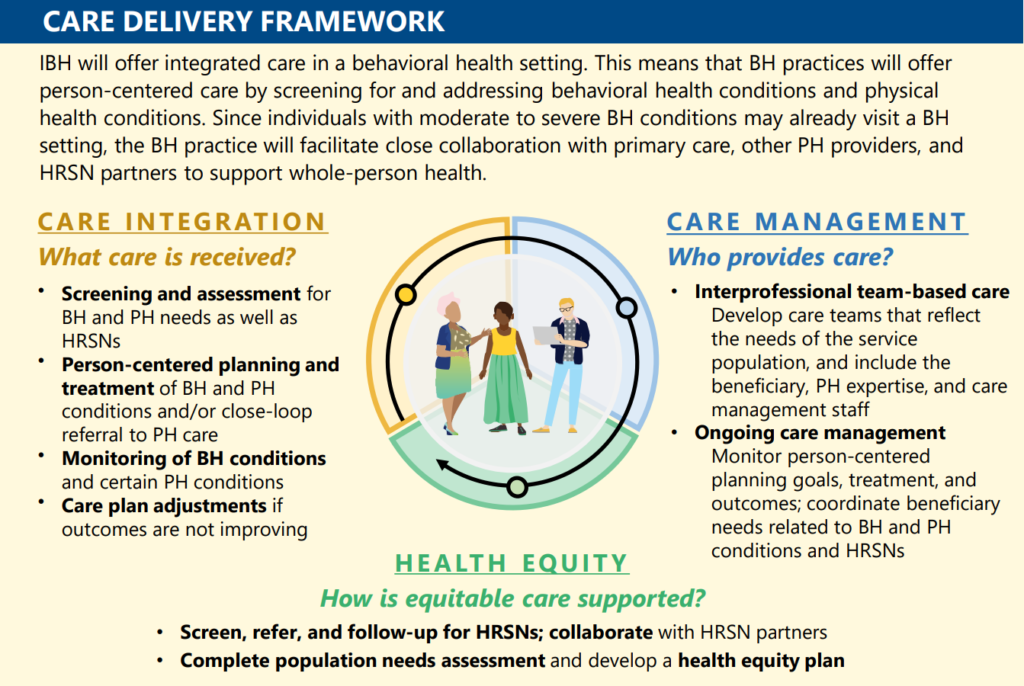
The IBH Model aims to bridge the gap between behavioral and physical health by:
- Empowering community-based behavioral health practices: These practices, including mental health centers, opioid treatment programs, and safety net providers, will become the central point of care, offering integrated services for both mental and physical health needs.
- Building interprofessional care teams: Behavioral health providers will lead teams encompassing primary care physicians, specialists, and community resources, ensuring coordinated care across the spectrum.
- Addressing health-related social needs (HRSNs): Screenings and referrals will connect patients with vital resources like housing, food, and transportation, addressing underlying social determinants that impact health.
- Value-based care: Practices will be compensated based on the quality of care and improved patient outcomes, incentivizing a focus on comprehensive, holistic well-being.
A State-Led Approach with Eight-Year Vision
The model will be implemented in eight states selected through a competitive application process. Participating states will partner with their mental health and/or SUD agencies and Medicaid Managed Care Organizations (MCOs) to develop and implement the IBH framework.
The eight-year journey will be divided into two phases:
- Pre-implementation (model years 1-3): This phase focuses on building capacity, recruiting practices, and establishing infrastructure. States and practices will receive funding for necessary upgrades in technology, staff training, and practice transformation activities.
- Implementation (model years 4-8): States will implement a Medicaid payment model that rewards practices for delivering integrated care, while selected practices can also participate in an additional Medicare payment model. Performance-based incentives will further encourage quality improvement throughout the implementation period.
Health Equity at the Core: Addressing Disparities
The IBH Model recognizes the disparities in health outcomes experienced by marginalized communities. To address this, it mandates:
- Health Equity Plans: Each participating practice must develop a plan outlining how they will address the specific needs of their diverse patient population and address any existing disparities in care.
- Screening and Monitoring for HRSNs: Regular screenings and referrals will ensure that patients receive the support they need to address social determinants affecting their health.
- Annual Assessments: Continuous monitoring of the model’s impact on health equity will be conducted to ensure its effectiveness in addressing disparities.
The Future of Integrated Care: Preparing for Advanced Models
The IBH Model is designed not only to improve care for individuals with dual mental and physical health needs but also to prepare practices for future advanced payment models and accountable care arrangements. This forward-thinking approach paves the way for a more integrated and equitable healthcare system, ultimately leading to better health outcomes for all.
“The Biden-Harris Administration believes that treating mental health and substance use disorder requires a “no wrong door” approach. This new model ensures that anyone can get access to the services they need, regardless of how they enter care,” said HHS Deputy Secretary Andrea Palm. “We will continue to test approaches that close the gaps between how behavioral and physical health are treated. Our goal is always to improve the overall quality of care and outcomes for patients and this model brings us one step closer.”
The model will launch in Fall 2024 and is anticipated to operate for eight years in up to eight states. CMS will release a Notice of Funding Opportunity for the model in Spring 2024.