What You Should Know:
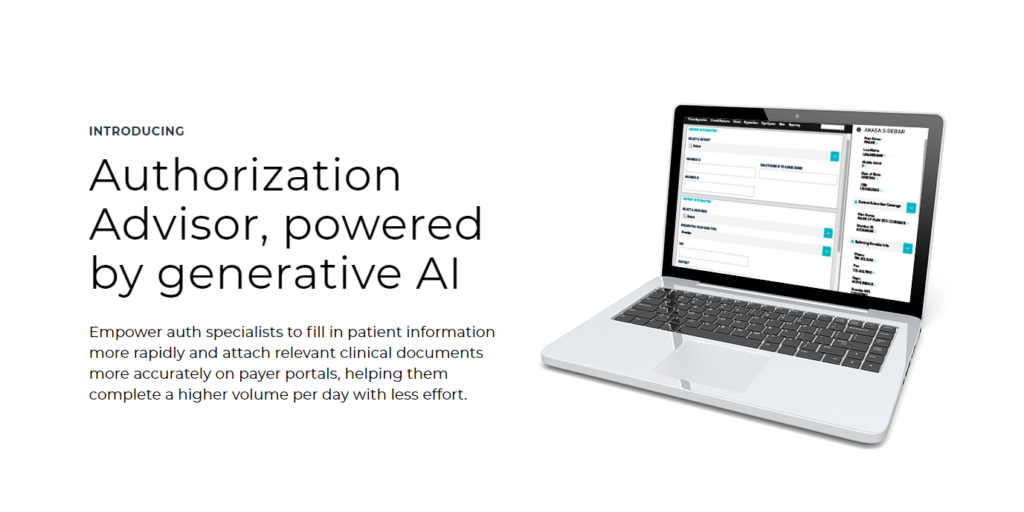
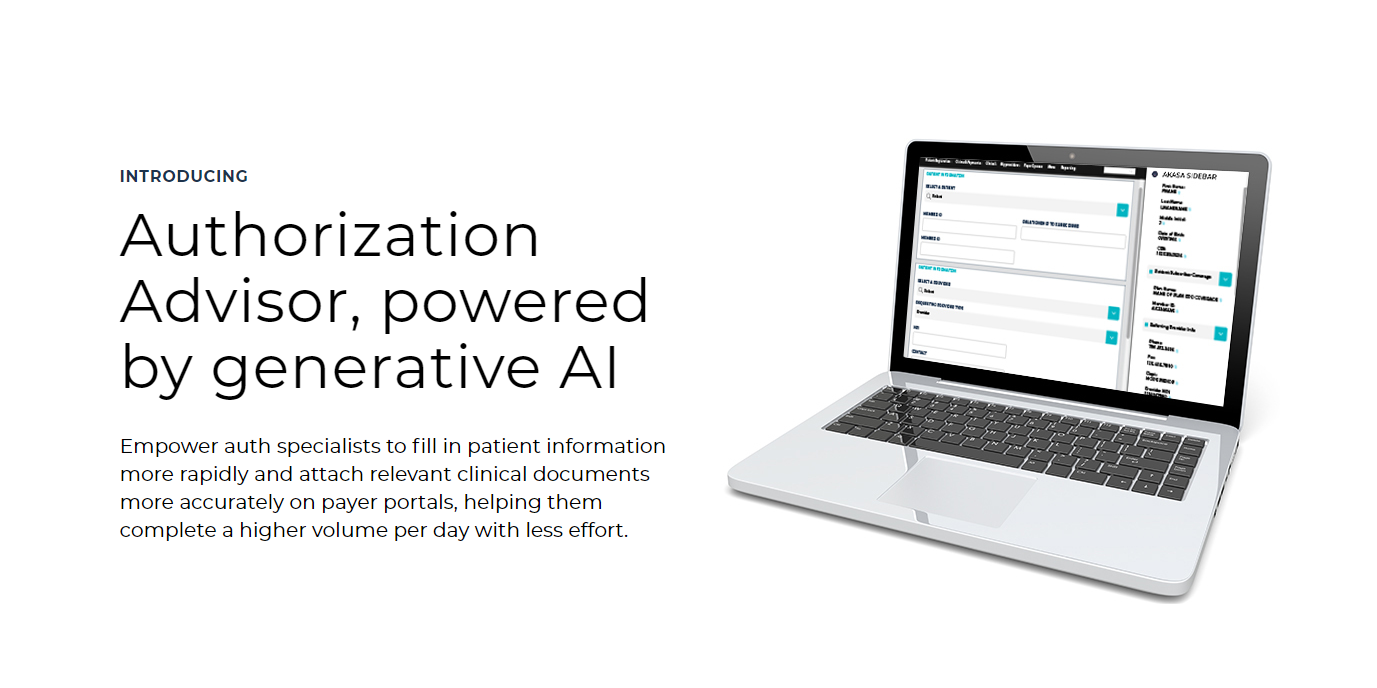
– AKASA, a leader in generative AI (GenAI) solutions for the revenue cycle, today announced the launch of Authorization Advisor™.
– Authorization Advisor tackles the time-consuming and error-prone process of prior authorization, a major pain point for healthcare providers.
Prior Authorization Made Easy with AI
Prior authorization, a process requiring approval from insurers before delivering certain services, is a significant burden for healthcare providers. It consumes a vast amount of time for revenue cycle teams and often delays patient care. Authorization Advisor tackles this challenge head-on, offering the potential to reduce authorization processing time by up to 50%. This innovative GenAI tool empowers prior authorization specialists with several key features:
- Interactive Sidebar View: Provides real-time access to patient details and curated clinical documentation directly within the payer portal workflow.
- Secure and Accurate Data Entry: Ensures patient information is filled out correctly on the payer portal.
- AI-Powered Document Recommendation: Recommends relevant clinical documents to support authorization requests, eliminating manual searches and improving accuracy.
- Reduced Manual Workload: Eliminates the need to sift through mountains of documents, freeing up valuable time for specialists.
Health System-Specific AI Model for Accuracy
AKASA’s unique approach utilizes a health system-specific AI model trained on an organization’s own clinical and financial data. This ensures the AI assistant understands the specific nuances of each healthcare system, unlike generic AI models. In fact, AKASA’s models have been shown to be 38% more accurate than generic versions when selecting relevant prior authorization documents.
By eliminating manual document searches and suggesting relevant supporting documentation, Authorization Advisor significantly reduces the administrative burden on patient access teams. This not only saves time but also helps ensure accurate authorization submissions, leading to faster approvals and improved cash flow for healthcare providers.
“Healthcare leaders are constantly trying to move any dial we can to have a positive impact on our people, processes, and patients,” said John Fox, former president and CEO of Emory and Beaumont Health, and advisor at AKASA. “AKASA is innovating in healthcare with these new generative AI tools. They’re at the right place at the right time to truly transform the revenue cycle by reducing friction and providing real results.”