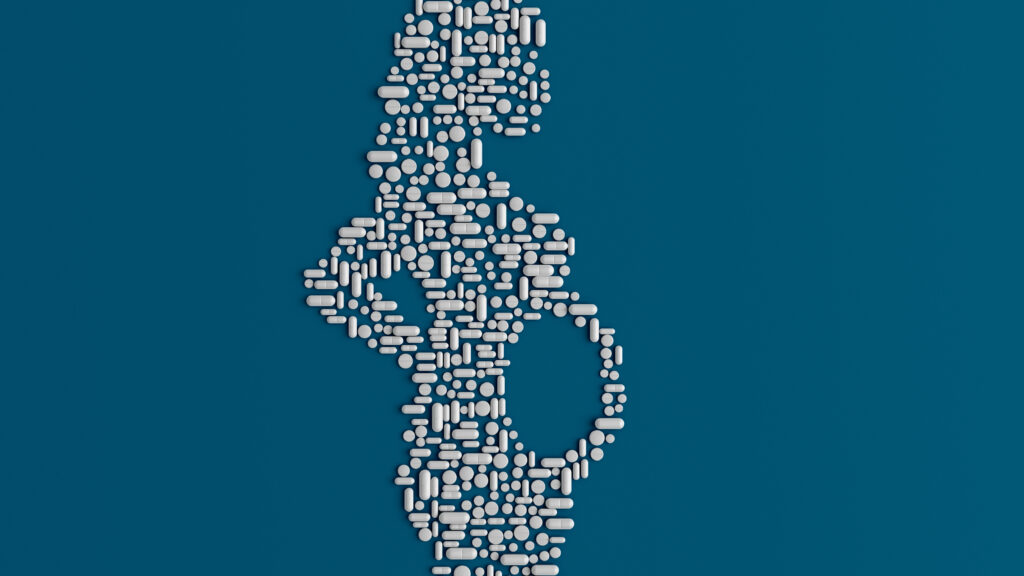
Imagine having to make this decision: Your health care provider recommends that you take a specific medicine for an illness or condition but then tells you it hasn’t been tested in people like you. Do you take the medication, or refuse it?
That’s the position the 3.5 million women who give birth each year in the U.S. are in when being counseled about taking medicines.
advertisement
Pregnant people have the same diseases as others, including depression, diabetes, high blood pressure, cancer, and HIV. And pregnancy can cause serious conditions that require the use of medicine. Up to 90% of pregnant people take one or more drugs during pregnancy, or were taking some kind of medication when they became pregnant.
Yet the clinicians who treat them nearly always have to tell them that information does not exist about the safety and effectiveness of these drugs for pregnant people and their fetuses. Human pregnancy data were available for just 11% of the medications approved by the FDA between 2010 and 2019. Without data, a clinician cannot be certain about whether the dosage of a drug needs to be increased or decreased to achieve the desired results, or assess whether the risk to the pregnant person and developing child would be greater if the mother’s condition is left untreated, since pregnancy alters the body in many ways, such as doubling blood volume and changing the way drugs are metabolized.
This information vacuum about the risks for pregnant people and their children has frustrated clinicians for years. Decades ago, medical quandaries of this sort arose for virtually all women, because most clinical research at that time was limited to men. Concentrated attention to this problem in the 1990s resulted in Congressional legislation and changes in Food and Drug Administration and National Institutes of Health policies that promoted women’s health through their increased participation in clinical research. But the situation for the subset of people who are pregnant remains unchanged.
advertisement
A report published this month by a committee of the National Academies of Sciences, Engineering, and Medicine, on which we served, offers a way forward.
Pregnant people understandably worry that the drugs they take might harm their fetuses. In the face of uncertainty, many decide not to take a medicine, or to stop taking it. That choice can have grave consequences for their well-being and even for maintaining the pregnancy. Others choose to take the medication, thus exposing themselves or their unborn children to uncertain risks of harm and no assurance of benefit.
Some pregnant people experience both horns of this dilemma. Our committee heard from a woman who was advised during her first and second pregnancies to stop all the medications she had been taking to control her rheumatoid arthritis. When her condition flared up during her second pregnancy, her doctors told her that the inflammation was more dangerous for her fetus than restarting the medication, which she did. Not surprisingly, she found that “a very uncomfortable and difficult decision to make” because of the limited safety data.
The usual explanation for excluding pregnant people from research is that pharmaceutical companies and other sponsors of clinical trials, and the research institutions and professionals who carry them out, fear being held legally liable for harming pregnant participants or their fetuses or children. Our committee found that such perceptions of legal risk are misplaced. In the past 60 years, there have been more than 1,000 reported legal cases associated with the post-market use of medical products in pregnancy, but no reported legal cases resulting from the use of investigational medical products by pregnant research participants.
Excluding pregnant people from research fails to prevent harm to them and their offspring — and actually increases it. Rather than producing data from carefully designed studies with a small number of closely monitored, consenting volunteers, excluding pregnant people from clinical trials creates a large experiment for use of a product by people in this population.
Use of the medication by pregnant people once it is on the market will not yield clinically useful information about the product’s dosage, effectiveness, and safety. Moreover, data are not systematically collected about the outcomes experienced by this population who decide to take a recommended treatment — or not to take it.
The exclusion of pregnant people from research extends to pregnancy-specific diseases. In the past two decades, the FDA has approved only one new medication for obstetrical conditions that remains on the market today. The harms that pregnant people and their fetuses experience aren’t usually attributed, as they should be, to the almost total failure to develop and test treatments for this population.
Many changes in attitudes about clinical research will need to occur if pregnant people are to have access to the medications they need and adequate evidence to make informed choices with the clinicians caring for them, something the rest of us take for granted.
Our committee recommends that the FDA accelerate that process by making clear that it expects pregnant women will be included as early as possible in the studies conducted for approval of any medical product that such patients are expected to use.
Congress should also pass legislation, similar to its 2003 legislation designed to incentivize research on pediatric drugs, to give the FDA the authority to require data on the dosage, administration, safety, and effectiveness of new medical products from research that includes pregnant people, as well as from post-marketing studies of existing products. To overcome challenges in implementing these changes, our committee recommends that Congress authorize programs to extend the time for which companies maintain the sole license for a drug, or provide tax breaks, when they promptly complete studies with pregnant participants and submit the data to the FDA for inclusion in product labels.
As others have advocated over the past three decades, the time has come to stop treating pregnant people as a vulnerable group that needs protection from research and instead to protect them and their offspring through research.
Alexander M. Capron is University Professor Emeritus at the University of Southern California and was the first director of the Department of Ethics, Trade, Human Rights and Health Law at the World Health Organization. Anna Mastroianni is a research professor in bioethics and law at the Johns Hopkins Berman Institute of Bioethics and Charles I. Stone Professor Emerita at the University of Washington School of Law. She was study director to the Institute of Medicine Committee on the Legal and Ethical Issues Relating to the Inclusion of Women in Clinical Research and coeditor of its 1994 report. They are both members of the National Academies of Sciences, Engineering, and Medicine’s Committee on Developing a Framework to Address Legal, Ethical, Regulatory, and Policy Issues for Research Specific to Pregnant and Lactating Persons, which released its report on April 10, 2024.