A biological, mechanism-based framework to reclassify multiple sclerosis (MS) types was proposed by the International Advisory Committee on Clinical Trials in Multiple Sclerosis.
The approach lays the groundwork for future consensus-based disease descriptions of MS that could transform drug discovery and improve patient care, the committee said.
“The rationale for the new framework was the increasing recognition that the classification of people with MS into distinct non-overlapping categories — i.e., relapsing-remitting, primary progressive, and secondary progressive — based on apparent course is artificial,” said framework co-author Jeffrey Cohen, MD, of the Cleveland Clinic in Ohio.
“Instead, the underlying biologic processes that account for relapses and the processes that cause progression appear to be present throughout the disease, to varying degrees over time, and to varying degrees in different people,” Cohen observed.
Developing a Biologically Based Framework
The proposed framework, presented by Tanja Kuhlmann, MD, of University Hospital Munster in Germany, and colleagues in Lancet Neurology, begins with recognition that MS is a disease that variably shifts between predominantly localized acute injury and widespread inflammation and neurodegeneration, coupled with failed compensatory mechanisms like neuroplasticity and remyelination.
Research has suggested that disability progression is not caused by one uniform disease mechanism but a combination of several mechanisms, the framework committee noted.
This means that MS can be considered a spectrum defined by relative contributions of overlapping processes. New understanding of key mechanisms underlying progression — and measures to quantify progressive pathology — will affect clinical care, treatment targets, and regulatory decision-making, they added.
The nuts and bolts will be mechanism-based results that can serve as markers of disease presence and activity in different dimensions. Assembling the appropriate measures for clinical- and research decision-making in individual patients will be a complex undertaking with several moving targets, the framework authors pointed out.
Disease marker reliability may change with age, for example. This — and the effects of biological sex, race and ethnicity, and other factors, must be accounted for — highlighting the complexity of re-conceptualizing MS as a combination of mechanisms such as non-resolving inflammation, neurodegeneration, oxidative stress, mitochondrial dysfunction, axonal degeneration, excitotoxicity, and failure of remyelination or neuroplasticity, which may vary and overlap in one patient.
The goal is to develop methods that quantify these mechanisms that could be applied in clinical trials and practice, the committee noted.
“The main implication is that disease therapies should target the biologic processes expressed by the person with MS, rather than an arbitrary disease category,” Cohen said.
Decades of Progress in MS
Since the turn of the century, the precise distinction between MS subtypes has become important because secondary progressive disease does not respond to most disease-modifying drugs approved for relapsing-remitting disease, observed Takashi Yamamura, MD, PhD, of the National Center of Neurology and Psychiatry in Tokyo, in a commentary about the framework proposal.
“Although there are many potential players in the pathogenesis of multiple sclerosis, including B cells, helper T cells, cytotoxic T cells, and microglia, the traditional framework for multiple sclerosis subtypes is indifferent to the pathogenesis,” he pointed out.
It’s become obvious that traditional MS subtypes do not represent the biological heterogeneity of patients, as shown by their heterogeneous microglia gene expression profiles, Yamamura added.
The ability to envision a new MS framework rests on two decades of progress in MS research, noted Bruce Cree, MD, PhD, of the University of California San Francisco, and co-authors, in a recent review.
In the past 20 years, there have been remarkable advances in MS, including a sea change in understanding the fundamental immune drivers mediating central nervous system (CNS) demyelination and neurodegeneration and the development of highly effective therapeutics, Cree and co-authors observed.
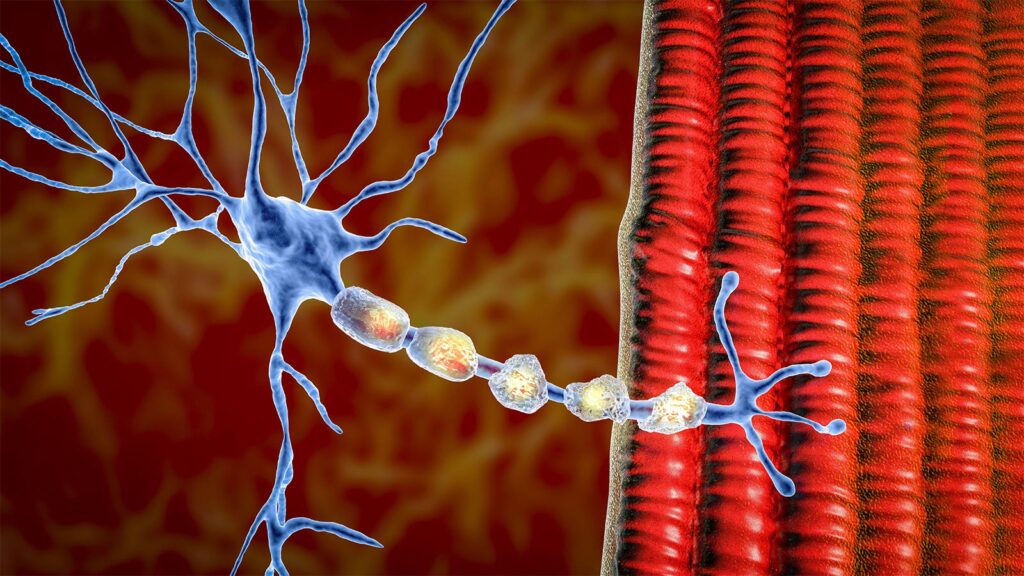
MS was long considered a T-cell mediated disorder, but researchers now recognize complex interactions between infiltrating immune system cells including B cells and CNS-resident cells, especially microglia and astrocytes, they noted. Importantly, B cells were recognized as key drivers of tissue damage, they added.
The two faces of MS — inflammation leading to relapses, and neurodegeneration mediating progression — represent a continuum across the course of the disease, Cree and colleagues said.
“From a clinical perspective, this promoted a unitary view, in which relapses and progression are considered overlapping features, with relapses mediated by B and T cells that move into the CNS from the bloodstream, and progression driven by diverse immune cells ‘trapped’ in the CNS and relatively resistant to peripherally administered therapies,” they wrote.
Next Steps Toward Reclassifying MS
Although the goal is distant and obstacles might arise, the time seems right to launch initiatives to reframe the classification of MS subtypes, Yamamura said.
Adopting biologically based definitions of progression will be challenging, as the existing descriptors are deeply embedded in clinical research and healthcare systems, the framework committee noted.
Patients rely on the descriptors to understand their disease journey and inform healthcare decisions. Regulatory authorities have used the descriptors, sometimes with complicated and differing interpretations, in MS treatment approvals.
“Until the underlying mechanisms and how they interact to drive progression are better understood, we expect that any new framework will require additional modification over time,” Kuhlmann and co-authors wrote.
A new framework will need to be integrated into clinical trials, clinical practice, and patient education, they pointed out. Developing a roadmap to implementing it will be an important focus of the International Advisory Committee on Clinical Trials in Multiple Sclerosis, they added.
Disclosures
The International Advisory Committee on Clinical Trials in Multiple Sclerosis work was jointly sponsored by the European Committee for Treatments and Research in Multiple Sclerosis and the National Multiple Sclerosis Society.
Kuhlmann reported relationships with the German Research Foundation, Interdisciplinary Centre for Clinical Studies Münster, National Multiple Sclerosis Society, European Leukodystrophy Association, Progressive MS Alliance, European Commission, Novartis, and Roche.
Cohen reported relationships with Biogen, Merck, Sanofi Genzyme, Novartis, Bristol-Myers, and Roche.
Yamamura reported relationships with AMED-CREST, Novartis, Chiome Bioscience, Biogen, Chugai, Alexion, Mitsubishi-Tanabe, and Takeda.
Please enable JavaScript to view the