Want to stay on top of the science and politics driving biotech today? Sign up to get our biotech newsletter in your inbox.
Hello! Today we learn whether AI might help hasten the development of n-of-1 therapies (hint: not yet), explore why the FDA hasn’t offered Orange Book guidance on drug-device combinations, and talk about CRISPR. A lot.
advertisement
The need-to-know this morning
- AC Immune has sold global licensing rights to an experimental immunotherapy for Alzheimer’s disease to the Japanese drugmaker Takeda. AC Immune received $100 million from Takeda for the therapy, called ACI-24.060, and is eligible for another $2.1 billion in future payments.
- Merck reported negative results from an interim analysis of a Phase 3 study involving the use of its experimental anti-TIGIT antibody as an adjuvant treatment for patients with high-risk melanoma.
- Cancer drug developer OnKure is going public via a reverse merger with Reneo Pharma.
AI might not yet help develop ‘n-of-1’ treatments
Can AI be used to help create “n-of-1” treatments for the rarest of genetic diseases? The jury’s still out, a new study suggests.
There’s been a wave of antisense oligonucleotide medications designed specifically to target the single mutation causing a patient’s symptoms. This is a compelling but time- and cost-prohibitive approach for most companies, which has led some, like Creyon Bio, to turn to artificial intelligence as a way to speed along the process.
Last week, Creyon said it successfully dosed a patient with a custom treatment that showed some signs of efficacy. What’s less clear, however, is whether machine learning helped make the drug faster or safer, STAT’s Jason Mast writes. Creyon said initially it would use AI to create the new medicine within seven months; instead, it took just over a year, which is no better than other n-of-1 approaches. Milasen, the first bespoke drug, took 10 months to develop. And Creyon’s drug didn’t cost “appreciably less” than other n-of-1 medicines, which run over $1 million to create.
advertisement
The FDA’s hands-off stance with drug-device combos
Drugmakers have long asked the FDA for clearer guidelines on how to list patents in a special registry called the Orange Book. This is important because it helps branded drugmakers inform generic competitors about their intellectual property. However, regulators haven’t offered the necessary guidance for drug-and-device combination products like inhalers and auto-injectors, STAT’s Ed Silverman writes. This is frustrating for industry players and patient advocates alike.
Recently, the FTC has stepped in, warning companies about improper patent listings in the Orange Book and taking legal action against those that try and extend their monopolies.
“The FDA needs to show some leadership and say which stuff won’t go in the Orange Book, but instead, they have been flip-flopping for years,” the leader of a nonprofit that focuses on pharmaceutical patent issues told STAT. “There is just too much uncertainty that hasn’t been cleared up.”
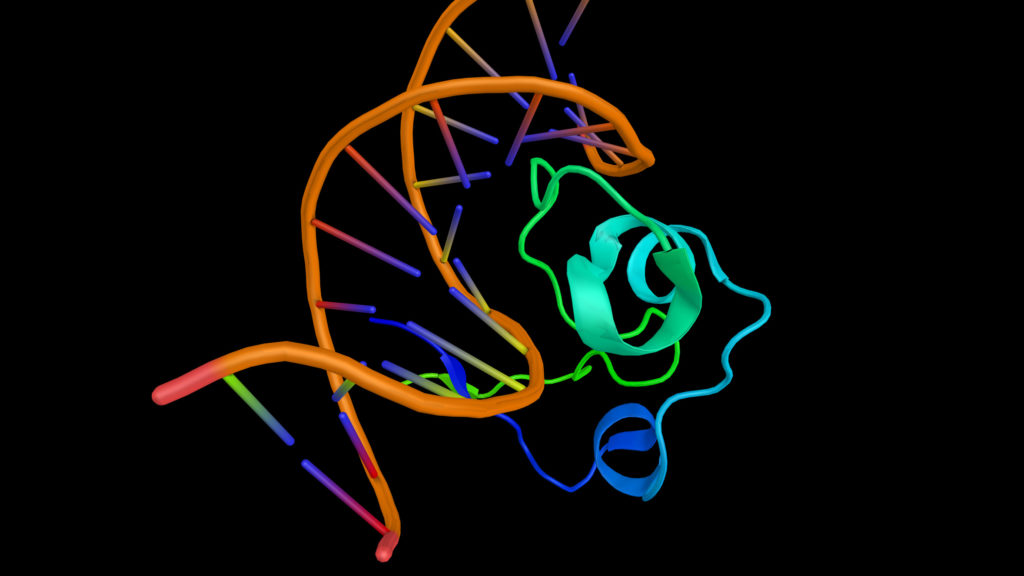
We now know Tome’s gene editing target
From STAT’s Jason Mast: For all the hype surrounding CRISPR, the tool has been largely effective at knocking out genes or making small edits. So when two scientists emerged a couple years ago touting technology capable of inserting large genes into human cells without doing major damage to the DNA, investors agreed to pour over $200 million to try to make it a reality.
That round, for Tome Biosciences, was announced in December. On Friday, at a major gene therapy conference, CEO Rahul Kakkar laid out for the first time how the company plans to use the technology: initially to treat a rare disease called phenylketonuria and to design a natural killer cell therapy heavily engineered to safely treat autoimmune diseases. Beyond that are plans to make a heart disease treatment and treatments for rare diseases homocystinuria and hemochromatosis.
The company will, of course, have competition. Tessera has also showed animal data for treating phenylketonuria with a gene editing system for changing individual letters. And Prime Medicine has a very similar technology for large gene insertion, though it has yet to reveal much detail on specific diseases.
A CRISPR approach did not cure HIV
An effort to use CRISPR editing to excise HIV from patient genomes did not work. A Phase 1 trial from Excision Therapeutics administered a CRISPR-based therapy to five patients with HIV. Researchers then took three of these patients off of conventional antiviral treatment, with hopes that they wouldn’t need to resume daily medication. But despite the CRISPR treatment, virus levels rebounded quickly.
This is likely because the gene editing approach wasn’t efficient enough, STAT’s Jason Mast writes. Excision used an adeno-associated virus to distribute the gene editing tool throughout the body — and AAVs don’t reach all cells. So even if the virus was excised from part of the body, it’s likely it lingered elsewhere.
But there were signs of hope: One patient’s infection didn’t rebound for about four months after stopping antivirals, whereas typically it comes back after three or four weeks. This suggests that CRISPR editing might ultimately be coupled with other approaches to cure HIV.
Maze gets another chance to partner on Pompe drug
Last year, Sanofi was set to pay $150 million in cash and stock to license an experimental Pompe disease treatment made by Maze Therapeutics — but the FTC blocked the deal and it fell through. Now, Maze has partnered with Japanese drugmaker Shionogi to further develop MZE001, again with $150 million up front, STAT’s Andrew Joseph writes.
Sanofi already sells two intravenous infusions for Pompe, which caused concern for regulators, who said an acquisition would extend Sanofi’s monopoly in the disease and dissuade competitors from entering the space. The French drugmaker walked away from the deal without personally informing the company: CEO Jason Coloma told STAT last year that he was “personally disappointed” in the Sanofi deal falling through.
“Shionogi has a track record of developing and delivering innovative medicines to patients worldwide, and we’re confident they are the right partner to continue to advance MZE001 through clinical trials so that it may reach patients with this life-threatening condition as soon as possible,” Coloma said in a statement.
More reads
- Pfizer and AstraZeneca announce new investments of nearly $1 billion in France, Reuters
- First person to receive a genetically modified pig kidney transplant dies nearly 2 months later, The Boston Globe
- ‘Pfizer for All’ consumer platform aims to provide post-Covid boost, Financial Times
- Harvard scientists unveil the most detailed map of the brain ever: ‘It’s an alien world inside your own head, The Boston Globe