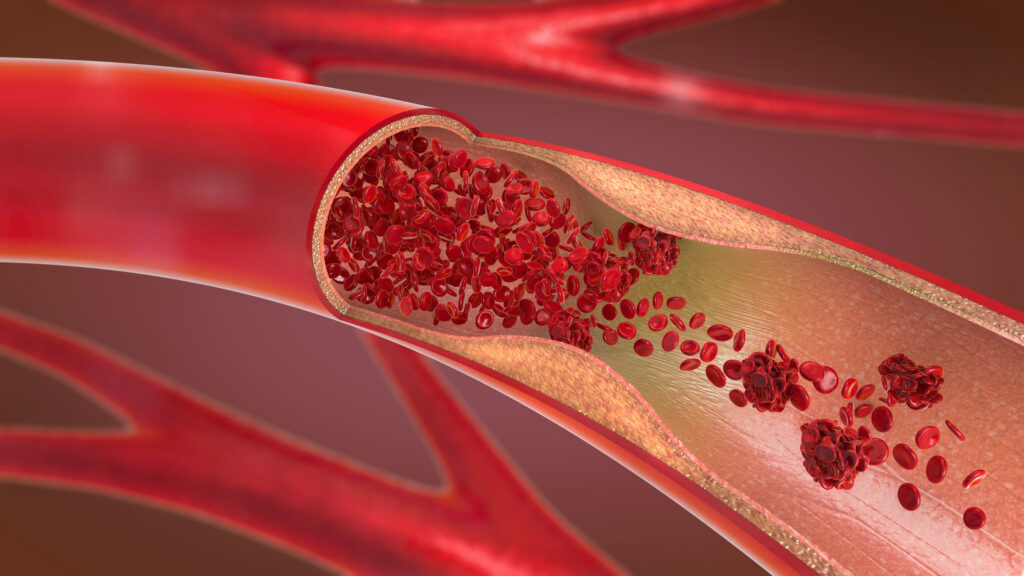
To better understand problems in the brain’s blood vessels that may lead to stroke, we need a better way to see them. Cardiovascular imaging can peer inside coronary arteries to spot clots blocking blood flow to the heart, but those tools are dangerously large for the smaller arteries inside the brain that twist and turn in tortuous ways.
Now researchers have designed a probe minuscule enough to fit inside the microcatheters that surgeons snake into cerebral arteries to place reinforcing stents or to scoop out clots. Their tiny probe delivered images from inside the arteries of 32 patients, detecting problems by illuminating the tissue and collecting back-scattered near-infrared light, based on a technology called neuro optical coherence tomography, or nOCT.
advertisement
The first-in-human study, published Wednesday in Science Translational Medicine, offers proof of concept for miniaturized, high-resolution visualization to see more clearly what’s going wrong and what to do about it.
“I think it’s an amazing technological achievement,” said Michael Levitt, a professor of neurological surgery and radiology at the University of Washington, who was not involved in the study. He’s been following optical coherence tomography, which was developed at the UW, primarily in ophthalmology to assess the thickness of the optic nerve. “The creation of catheter-based OCT was one of these things that I personally always thought was like, wow, this is really cool — but. It was always hard to think about how to use that technology in the brain.”
That’s because the brain is hard to reach and its thin, sensitive arteries curl and curve so much that cramming something stiff inside them can cause severe damage.
advertisement
Today, neurologists glimpse the vessel wall only from the outside, with X-rays using contrast medium to show their shape. “Everything they see with the X-rays is a shadow of the vessels,” study senior author Giovanni Ughi told STAT. “We created this tiny, small probe, which is like a microscope you can bring inside the arteries, and look at them directly for the first time.”
Ughi is senior director of advanced development at Spryte Medical, a Bedford, Mass., startup developing the nOCT device, and also an assistant professor of radiology at UMass Chan Medical School in Worcester, Mass. The study was funded in part by the National Institutes of Health. It followed bench experiments and animal studies.

There have been previous efforts to repurpose cardiac or peripheral vascular OCT to try to reach the brain. But because those tools have been large and stiff, Levitt said he’s been too nervous to try them, despite their promise of better views. “It’s hard to imagine using the existing technology for that purpose because of the risk,” he said.
The patients included in the new study had a variety of problems in their brains, including aneurysms, which are bulges in the vessel wall that can rupture; ischemic stroke, when a blood clot blocks blood flow; arterial stenoses, when plaque from fats and cholesterol narrows the vessels; dissections, when the artery’s lining tears; and atherosclerosis, when plaque builds up. To see inside these vessels, the researchers created a probe that would fit inside the hollow microcatheters, which measure 0.03 millimeters, or about seven times the width of a human hair, and can ferry stents or wires.
The probe itself carries an optical fiber that is about only about one human hair wide, along with an optical lens using laser light in what adds up to a very tiny, very high-resolution camera. Ughi envisions the probe being used as a diagnostic tool at many points in caring for a person with cerebrovascular disease. X-rays before and during any procedure offer an incomplete, two-dimensional picture, but the new probe could bring three-dimensional clarity before, during, and after a procedure.
“It can be an important clinical tool,” Ughi said. “It can also be important for clinical research of new drugs or new devices.”
Levitt calls it a paradigm change.
“It almost sounds trivial, like, you know, congratulations,” he said. “You just took this thing and made it smaller, but actually, that’s really how you win the game, right? The technology is of no use if you can’t deliver it where it needs to go — and where it needs to go is a small and delicate artery.”
For Spryte Medical, the next step is to work with the Food and Drug Administration and regulatory bodies in Europe, Japan, and elsewhere to gain clearance to market the probe.
For surgeons, the tool can potentially inform diagnoses, guide treatments, and provide quality assurance checks on stent placement or clot removal, for example. For scientists, the paper has generated hypotheses that need to be tested to see how this technology might improve current treatments, including drugs and devices.
“Intravascular imaging has helped many, many other fields in medicine, but it’s not available yet for neurology,” Ughi said. “The scope and the goal of our work is to bring intravascular imaging to try to help neuroendovascular as a field to advance. That’s really the mission.”
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.