HIV has long stumped immunologists looking to develop an effective vaccine. All of the most promising approaches pioneered in the past three and a half decades have ultimately failed, and only a few months ago, the last trial expected to potentially deliver a vaccine within this decade was shut down.
But HIV scientists are nothing if not resilient, and used to trying one new approach after another. One of the latest and most promising centers around teaching the immune system to produce powerful and protective antibody responses through exposure to a series of different vaccine molecules. Researchers are already beginning to test this strategy in people, and on Thursday the strategy gained additional support from a set of four studies published in Science, Science Translational Medicine, and Science Immunology.
advertisement
The studies, conducted in mice and monkeys, showed that researchers could begin to shepherd immune cells toward producing antibodies that block a broad swath of viral strains — an important first step.
“In my career with vaccines, it’s never felt like we’ve been closer to the understanding of how to make an effective HIV vaccine and to make the tangible steps necessary to get there,” said James Kublin, executive director of the HIV Vaccine Trials Network, who was not involved in the new research.
That optimism is tempered by the reality that the history of HIV vaccine research is riddled with failure. In 1984, Margaret Heckler, secretary of the Department of Health and Human Services, declared that she was hopeful researchers would develop a vaccine within two years. Instead, scientists have been thwarted at every turn. Merck famously suspended a trial after evidence suggested that people who’d been immunized might be more likely to get infected. Johnson & Johnson halted a trial in 2021, and last December a study that experts called “the last roll of the dice” for a vaccine before the 2030s stopped after a data monitoring committee determined there was virtually no chance the shots would work.
advertisement
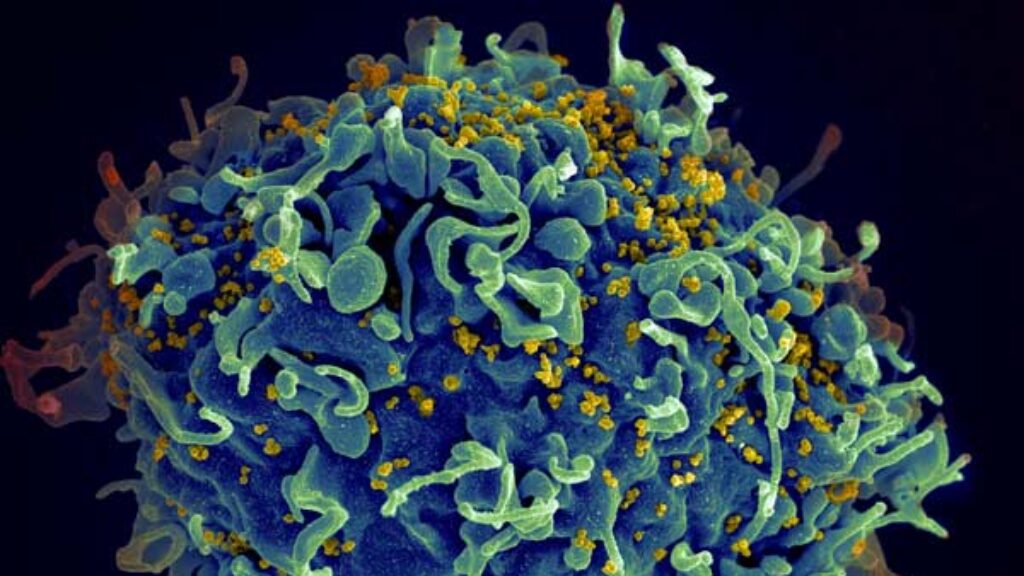
One of the central issues is that HIV is a shapeshifter: The virus’s genetic code mutates at the highest rate known to science. That makes it difficult for infected people to produce a protective immune response. About a fifth of patients produce so-called broadly neutralizing antibodies, which latch onto a wide range of strains and prevent the virus from slipping inside human cells. But it typically takes a couple of years for people to produce these antibodies, at which point they already have an established and chronic infection.
A vaccine that elicits broadly neutralizing antibodies before infection could be transformative; despite advances in HIV treatment, more than 600,000 people died of AIDS last year. But there are a few reasons turning that goal into a reality will be difficult. Antibodies are produced by immune cells known as B cells, and the B cells that have the potential to produce broadly neutralizing HIV antibodies are exceedingly rare. While a regular vaccine targets about 1 in 1,000 B cells, a vaccine trying to activate a broad HIV response would have to hit cells as rare as 1 in 1 million or more, said Shane Crotty, a professor at La Jolla Institute for Immunology and an author on the study in monkeys.
“In most vaccines, you’re trying to get a common antibody response, it’s kind of like if there’s a jar of jelly beans and it has one gold — and that’s the one you’re trying to get,” said Crotty. “But for a hard problem like HIV, instead of a jelly bean jar, you’re trying to find that one gold jelly bean in a swimming pool.”
Another challenge is that these B cells don’t actually produce broadly neutralizing responses at first. Instead, these cells mature by going through a rapid cycle of mutations concentrated in antibody-coding genes. That has led researchers to come up with a vaccine strategy that relies on a series of different immunogens that guide B cells toward producing a broadly neutralizing response.
In one of the recent studies, a team led by scientists at Scripps Research Institute reported success with the first part of this process — selectively activating rare B cells and beginning to guide their maturation — in all eight rhesus macaques examined. Researchers used proteins engineered to activate only those B cells with the potential to produce broad responses. They found that the antibodies produced by these cells latched onto the virus in a way that resembled a known broadly neutralizing antibody isolated from a patient. But the team of authors didn’t show whether these antibodies protected against infection and disease.
The results are both encouraging and many steps removed from effective vaccines in people’s arms. “Because these cells are so incredibly rare, many people have just said this is impossible. And we’ve shown it definitely is possible, and it happened in every single animal that we tried it in. It was really a phenomenal outcome,” said Crotty. “That first step is extraordinarily hard, and we think the subsequent steps might be easier — not easy, it’s still a hard problem, but easier.”
Two of the other new studies tested guiding B cells toward producing antibodies that latch onto a part of HIV known as the CD4 binding site, a region with minimal differences between strains because it’s essential for infection. These studies, conducted in mice modified to more closely resemble the human immune system, showed that researchers could use an initial molecule to activate rare B cells and could then follow up with a second mutation that guided the immune cells much closer to producing a broadly neutralizing response against the CD4 binding site. Another mouse study produced similar results but was focused on targeting a different region of the HIV surface known as the V3 glycan epitope.
While the macaque study showed the B cells can be primed to produce the right response, the mice studies are “a step further in showing that we can actually give a booster immunogen and drive those responses in the direction we want,” said Christopher Cottrell, a researcher at the Scripps Consortium for HIV/AIDS Vaccine Development and lead author of one of the mouse studies.
The following steps will be tested in mice that have been modified to already have the immune response triggered by the primer — this will save researchers the six months that regular mice would need to develop immunity after the injection.
That something worked in macaques and mice doesn’t mean it will in people. But preliminary results announced in 2021 from a Phase 1 trial found that 35 of 36 study participants produced an initial immune response to a candidate vaccine targeted toward B cells with the potential to produce broad responses. A follow-up trial is now underway at the HIV Vaccine Trials Network to see if researchers can push B cells further toward making broadly neutralizing antibodies, with results planned to be available next year.
Should that be successful, researchers would begin a long and complicated process to move from targeting these cells to polishing their abilities through subsequent, targeted vaccination. “There’s still multiple steps on the path,” said Crotty, but the targeted cells have the right characteristics to produce the broadly immunizing antibodies that are needed for protection against the virus. “It looks very different than any previous HIV vaccine strategy or clinical trials,” he said.
It’s not the first time people in HIV research have thought that they were onto something new. And even if all goes according to plan, it’s hard to know when a human vaccine could emerge.
But if the approach fails, researchers won’t consider it a wasted effort: The road of vaccine innovation is paved with failed HIV vaccine attempts. Protein stabilization methods and mRNA platforms were initially developed to stop a virus that continues to elude the most imaginative immunization approaches.
Advances from this work could improve our ability to immunize against longstanding public health foes such as malaria and tuberculosis, or the flu, or even the next, yet unknown, pandemic, said Kublin. And it could help beyond viruses, for instance in immunotherapy applied to some types of cancer. “There are all of these collateral benefits from this work that will improve health,” he said, “not only for infectious diseases but noncommunicable diseases as well.”