A few years ago, the Centers for Medicare and Medicaid Services launched a big experiment. The agency wanted to see if financial incentives and penalties would improve care for people with end-stage kidney disease. So far, it hasn’t worked, a new study finds.
The End-Stage Renal Disease Treatment Choices (ETC) model is a historic effort, both because it’s the largest such experiment in the history of American health care and because, unlike previous CMS Innovation Center pilot programs, it’s mandatory. About 30% of dialysis providers in the country participate, while the other 70% are used as a control group. It’s shaped like a gold-standard, randomized control trial, and run by the entity that covers the majority of health care related to end-stage renal disease, including dialysis.
advertisement
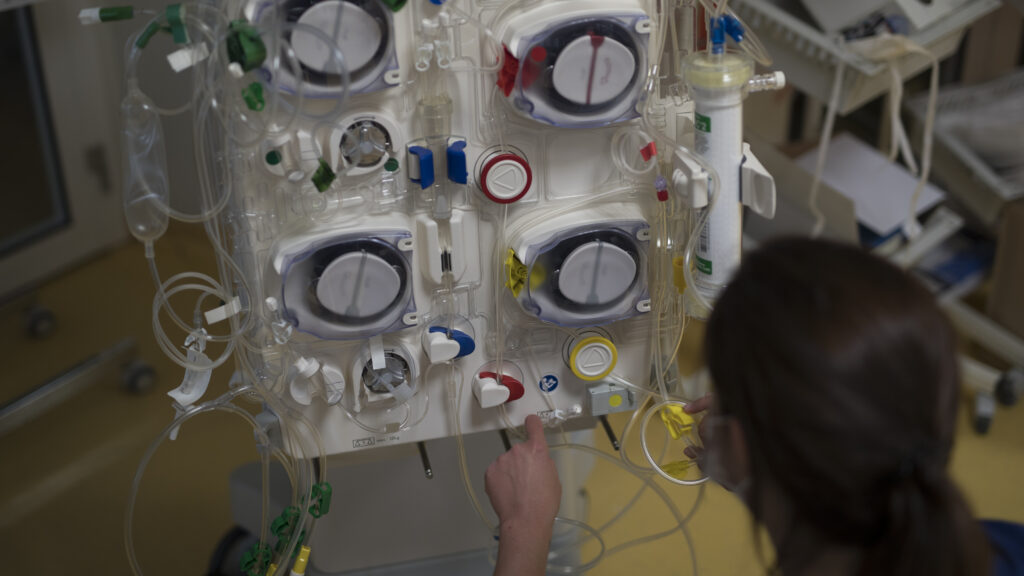
Each year, providers are graded on how many patients they can move to home dialysis, which is more affordable for the health care system, and how many people go on to receive kidney transplants, among other metrics. If they do well, they receive some extra money. Those who don’t do well face financial penalties. Both amounts increase with each year of the experiment, up to an 8% bonus or 10% penalty by the end of the program.
STAT+ Exclusive Story
Already have an account? Log in

Get unlimited access to award-winning journalism and exclusive events.