The FDA’s recent expanded approval of delandistrogene moxeparvovec (Elevidys) widened access to the gene therapy to include ambulatory and non-ambulatory Duchenne muscular dystrophy patients ages 4 and older with a confirmed DMD mutation.
In June 2024, the FDA converted its previous accelerated approval to traditional approval for ambulatory Duchenne patients ages 4 and up, and granted accelerated approval for non-ambulatory Duchenne patients in that age group.
Expanded approval came even though the treatment failed to meet its primary endpoint in a phase III trial. Despite this, “the FDA found the observations regarding the secondary endpoints and exploratory endpoints to be compelling and to indicate clinical benefit compared to placebo,” the agency said in a statement. “These endpoints include improvements in time to rise from the floor, 10-meter walk/run, time to ascend four steps, and creatine kinase levels.”
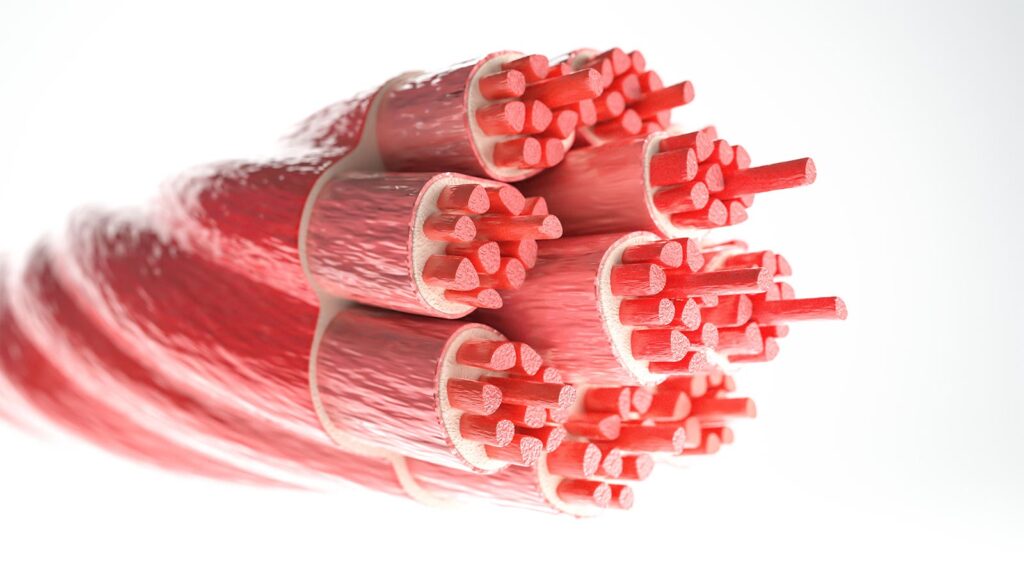
In Duchenne muscular dystrophy, a DMD mutation leads to a lack of dystrophin protein, causing muscle weakness and atrophy.
“Delandistrogene moxeparvovec was engineered to retain the essential components of the DMD gene — the largest gene in the body — while also making it small enough to fit into an adeno-associated viral vector for delivery to muscle,” Jerry Mendell, MD, an advisor to Nationwide Children’s Hospital in Columbus, Ohio, and Sarepta Therapeutics, told MedPage Today.
The treatment is administered in a single intravenous dose. The vector enters the muscle cell nucleus and releases the genetic material — the promoter and the delandistrogene moxeparvovec transgene, said Mendell. This forms a stable circle of DNA, or episome, used to generate the mRNA which is then translated into micro-dystrophin protein, smaller but more functional than the dystrophin produced with DMD mutations. The protein ultimately localizes to the muscle cell membrane.
“In studies of more than 200 Duchenne muscular dystrophy patients, muscle biopsy analyses have confirmed that treatment with delandistrogene moxeparvovec leads to expression of micro-dystrophin in skeletal muscle,” Mendell noted. “In addition, functional outcomes support that delandistrogene moxeparvovec modifies the trajectory of Duchenne, demonstrating a treatment benefit that is clinically meaningful.”
Not all Duchenne patients are candidates for delandistrogene moxeparvovec, based on their adeno-associated virus (AAV) antibody status and their mutation, Kevin Flanigan, MD, of Nationwide Children’s Hospital, emphasized. The treatment is contraindicated in patients with any deletion in exon 8 and/or exon 9 in the DMD gene.
“It is important to be mindful of the risks to patients — particularly the minimal information [available] about risks to larger, older boys — as well as the limitations to understanding the efficacy and durability of this treatment,” Flanigan told MedPage Today.
“We make certain to counsel parents that not all children may respond equally,” he continued. “For the moment, we are likely to prioritize treatment in younger boys, where efficacy and safety data are more complete. We encourage all sites who intend to deliver the vector to understand the significant follow-up and monitoring requirements needed to ensure patient safety.”
Screening and Monitoring
In a recent review published in Pediatric Neurology, Mendell and co-authors summarized practical considerations before and after delandistrogene moxeparvovec administration.
Before infusion, the group recommended screening for anti-AAV rhesus isolate serotype 74 total binding antibody titers less than 1:400; ensuring up-to-date vaccinations and avoiding vaccine co-administration with infusion; checking liver function and postponing infusion if liver disease or any infection is present; and starting additional corticosteroids 1 day pre-infusion for patients already on corticosteroids.
Post-infusion, they advised weekly monitoring for liver function tests (3 months), troponin-I (4 weeks), and platelets (2 weeks). They also recommended maintenance of the corticosteroid regimen for at least 60 days post-infusion, unless earlier tapering is indicated.
In 2024, an expert panel led by Craig Zaidman, MD, of the Washington University in St. Louis, published a paper in the Journal of Neuromuscular Diseases about managing adverse events after delandistrogene moxeparvovec treatment, including vomiting, acute liver injury, myocarditis, and immune-mediated myositis (IMM).
The panel suggested laboratory tests 1 month prior to infusion, and again within 1-3 days of infusion, to establish a patient’s baseline health status and evaluate liver and heart function.
Vomiting was the most frequent treatment-related adverse event reported in clinical studies, which raised concerns about the ability to tolerate the oral corticosteroids used to suppress responses to the viral capsid. Parenteral steroid administration may be necessary, the panelists noted. All patients with elevated liver enzymes require more frequent lab monitoring and, in moderate or severe cases, increased corticosteroids and additional evaluation, they added.
Increases in troponin I also were reported, and the panel considered several scenarios. An asymptomatic patient with mildly elevated troponin I could be evaluated in-person and have more frequent lab monitoring, they suggested. Symptomatic patients should be hospitalized, receive intravenous corticosteroids, a cardiology consultation, and consideration for intravenous immunoglobulin (IVIG).
Presentation of IMM was variable, including rapidly progressive axial, appendicular, and respiratory weakness; bulbar weakness; and swelling related to angioedema. A patient with possible IMM should be hospitalized, 67% of the panel suggested, and baseline lab collection should be repeated within 2 to 5 days (92% of the panel). Patients with swallowing or chewing difficulty, especially bulbar weakness, should have a swallow study (67%) and neuromuscular strength assessment (92%). An echocardiogram and electrocardiogram should be done. An increase in corticosteroids should be tried and, if rapid improvement does not occur, adding plasmapheresis, IVIG, or other targeted immunosuppressive therapy should be considered.
The panel convened before the FDA approved delandistrogene moxeparvovec and the report was based on experiences until October 2022. “These findings, based on clinical trial experience and individual health care provider experience, address the limited data available regarding management of safety issues arising post-delandistrogene moxeparvovec administration,” the panelists acknowledged.
Disclosures
Delandistrogene moxeparvovec studies were funded by Sarepta Therapeutics.
Mendell reported relationships with Sarepta and was a co-inventor of AAVrh74.MHCK7.micro-dys technology. Nationwide Children’s Hospital holds the patent for the vector.
Zaidman reported relationships with Sarepta, Optum Therapeutics, Biogen, and Novartis.
Please enable JavaScript to view the