Until the early 20th century, America regularly experienced brutally destructive urban fires. Conflagrations like the 1871 Great Chicago Fire, which destroyed more than 17,000 buildings and left 100,000 people homeless, were thought to be unfortunate but inevitable: Large numbers of buildings in close proximity naturally led to large fires.
But then, conscious changes to the built environment eliminated large urban fires. Cities adopted building codes that restricted the use of flammable materials. New buildings incorporated fire doors, fire escapes, automatic sprinklers, fire alarms, and other safety features. By changing the way we build our buildings and infrastructure, we’ve quenched a significant threat to public health and safety.
advertisement
Today, we face a similar opportunity to eliminate a health risk once thought inevitable: poor air quality in indoor spaces. Dirty air leads to all kinds of harms: pathogen transmission, high CO2 levels that worsen cognitive function, and particulates that cause respiratory issues. Like urban fires, getting sick from shared air has been generally assumed to be inevitable, a feature of living in proximity to other people. But it’s not. In the same way that stricter building codes and other built environment changes ended large urban fires, targeted changes in indoor air requirements could prevent (or at least constrain) future pandemics, reduce seasonal infections, and improve public health.
Humans spend 90% of our time indoors, where air circulates less well and a wide range of contaminants build up. These contaminants have measurable negative effects on our health and well-being. For instance, it’s increasingly clear that we think better in less polluted air, particularly air with less CO2. A Harvard study found cognitive function scores were 61% higher in indoor spaces with increased ventilation compared with a conventional building. Some critics have wondered whether that effect size will replicate. But similar results abound across a wide range of contexts: In high CO2 environments, chess players blunder more, American and British students score worse on tests, and office worker productivity declines.
Pathogen transmission indoors may be the more salient example, as Covid-19 made aerosol inhalation a widely understood phenomenon. All pathogens that can be transmitted person-to-person tend to do so indoors, as outdoor aerosols become quickly diluted, or “inactivated” by UV radiation in sunlight. Viruses are particularly ill-suited to surviving outdoors but spread quickly indoors. Almost all our respiratory disease transmission happens inside.
advertisement
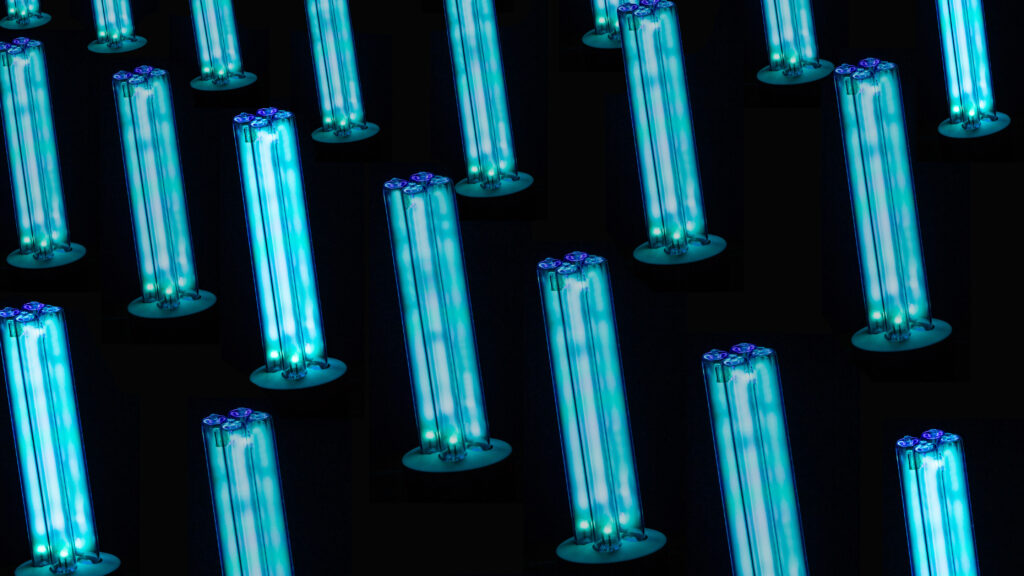
Currently, almost all buildings in the U.S. use some combination of ventilation and filtration to clean indoor air, but very few take advantage of disinfection to inactivate pathogens in the air directly. While ultraviolet (UV) light is the most widely used and promising method of disinfection, it’s also harmful to humans. As a result, it’s mainly used for pathogen disinfection in specific health care settings, or in contexts where high ceilings allow for upper room use.
But a novel technology known as far-UVC could prove far more effective at disinfection. Whereas conventional UVC has a wavelength range of 254 nanometers, far-UVC’s wavelength range is shorter at 200-230 nanometers and can’t penetrate beyond the outer layer of dead skin cells, or the tear layer of the eye. As a result, it can inactivate airborne and surface pathogens without harming human tissues. Far-UVC has effectively inactivated a wide range of pathogens in laboratory studies, including bacteria (like Staphylococcus aureus) and viruses (like influenza A virus and SARS-CoV-2).
Recent studies suggest far-UVC light can clean air of pathogens incredibly quickly, without any harm caused to humans. If we can support more research into far-UVC’s efficacy and find ways to implement it globally, we have the chance to significantly mitigate the impact of the next pandemic, while generating a wide range of benefits to everyone who spends regular time indoors.
Defeating major urban fires required a combination of new technologies and new building standards. We’ll need both to improve indoor air quality. But while technologies like far-UVC hold promise, our building codes and standards have limited effect on indoor air quality and often don’t refer to CO2 or pathogens at all. The only legally enforceable federal indoor air standards limits are set by the Occupational Safety and Health Administration, and these regulations are outdated and inadequate by OSHA’s admission.
To effectively tackle the issue of indoor air quality, we suggest a multi-modality approach: ventilation to decrease CO2, filtration to reduce particulates (especially important if we are to face more wildfires because of climate change), and far-UVC for disinfection. This comprehensive approach can address a broad spectrum of air quality concerns, ensuring healthier indoor environments.
Buildings in the U.S. largely follow standards set by the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), which just approved a new Control of Infectious Aerosols standard. In a new paper, we outline how this new standard can be leveraged alongside improvements to existing standards to encourage building operators to control CO2 and pathogens could improve indoor air quality.
This won’t be cheap. Building standards are implemented at the state and local level, are updated infrequently, and are subject to political pressure from interest groups that oppose expensive mandates. This will necessarily slow widespread adoption of stricter air quality standards.
However, because indoor infections are most likely to occur in a small number of high-occupancy buildings, significant benefits in public health can be achieved without universal adoption. An estimate produced for the U.K. Royal Academy of Engineering found that by simply improving the HVAC systems with existing available technology of the 5% of buildings most likely to cause infections, airborne infections would be reduced by 17%. And while the costs of interventions like far-UVC are as of yet unknown, significant benefits can be gained for relatively minor costs and can be implemented by building owners today. A Harvard study estimated that increasing ventilation in commercial buildings to double the current code minimum would cost on the order of $40 per occupant per year, but would have $6,500 in benefits from increased worker performance, even before taking into account the benefits from reduced infections.
State and federal incentives to adopt stronger air quality standards could start by focusing on large, public indoor spaces with high throughput, like indoor stadiums, train stations, and airports. Future incentives could focus on new construction and major renovations, rather than retrofitting existing buildings.
Today, the risk of fire death in the U.S. has fallen by roughly 90% since 1920, and the fires that do occur are almost all limited to their floor or room of origin. Denizens of major American cities in the late 19th century would find this progress unbelievable. By tackling the contaminants in indoor air, we have the opportunity to defeat another public health menace.
Juan Cambeiro and Brian Potter are fellows at the Institute for Progress, a nonpartisan research and advocacy organization dedicated to accelerating scientific, technological, and industrial progress.