Expansion of treatment options for axial spondyloarthritis (axSpA) has brought attention to documented delays in diagnosis, which is estimated to be an average of 6.7 years worldwide.
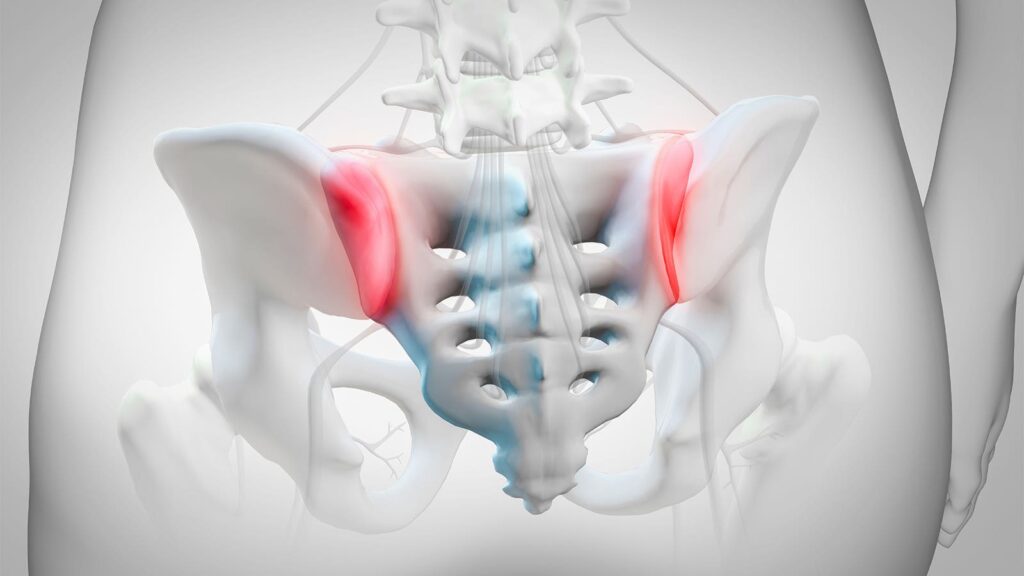
Spondyloarthritis (SpA) has two forms: axSpA, which affects the spine and sacroiliac joints predominantly, and peripheral SpA, which affects the peripheral joints. Manifestation of axSpA can be either radiographic axSpA, which is synonymous with ankylosing spondylitis, or non-radiographic axSpA.
Guidelines present criteria for classification of SpA for patients with chronic back pain (3 or more months) and an onset younger than 45 years. These include sacroiliitis on imaging, especially in the presence of human leucocyte antigen B27 (HLA-B27).
Rheumatologists face challenges when diagnosing axSpA, said Elaine Husni, MD, MPH, of the Cleveland Clinic in Ohio.
“Clinical features such as inflammatory back pain, HLA-B27 status, and extra-spinal manifestations are important but not definitive on their own,” Husni told MedPage Today.
“The specificity of these features can be lower than previously assumed, and their presence does not always lead to a diagnosis of axSpA,” she continued. “Additionally, the heterogeneity of symptoms and the presence of non-radiographic axSpA complicate the diagnostic process, as these patients may present with normal x-rays but still have significant disease.”
An important issue is the lack of validated diagnostic criteria and the misuse of existing classification criteria, which can lead to overdiagnosis, misdiagnosis, and underdiagnosis, Husni added.
Imaging interpretation is another challenge. “There is substantial inter-reader variability in interpreting MRI and x-ray images, and the radiologic definitions of axSpA are continually being refined to improve diagnostic accuracy,” she said.
How Delays Affect Patients
A delayed axSpA diagnosis can affect a patient in multiple ways. Compared with axSpA patients with earlier diagnoses, those with delayed diagnosis generally had higher disease activity, worse physical function, and more structural damage, a meta-analysis found. They also had a greater likelihood of work disability, higher healthcare costs, and a greater likelihood of depression, negative psychological impacts, and worse quality of life.
A diagnostic delay of 2 to 6 years may be typical in axSpA, noted Raj Sengupta, MBBS, of the University of Bath in England, and co-authors in a recent review. “This time span presents a window of opportunity for earlier diagnosis and intervention, which will likely improve patient outcomes,” they wrote.
Evidence shows shortcomings at both primary and secondary care levels that contribute to delayed diagnosis, Sengupta and colleagues pointed out. Most (62%) patients reported contacting a healthcare practitioner in the first year they developed axSpA symptoms, they noted.
“Despite the existence of various published guidelines for appropriate referral and investigations in patients with chronic lower back pain, recommendations are not always implemented in clinical practice, especially referral for appropriate imaging when axSpA is suspected,” they wrote.
The European Map of Axial Spondyloarthritis (EMAS) study showed a greater delay to diagnosis in female patients, “which may be due to possible bias from physicians (ankylosing spondylitis historically thought of as a predominantly male disease),” or a different pattern of clinical presentations across genders, as females typically had more arthritis than enthesitis-related symptomatology and were less likely to test positive in HLA-B27 testing or on imaging, Sengupta and co-authors noted. “It is thus crucial to sensitize physicians to gender differences in axSpA.”
In 2024, the SPACE study showed axSpA can be diagnosed quickly in many patients if they are referred to a rheumatologist early. In an overall cohort of 552 chronic back pain patients who had a prompt (within 2 years) referral to a rheumatologist, 32% were diagnosed with definite axSpA at baseline.
“Most patients can be unequivocally and reliably diagnosed at their first assessment,” reported Mary Lucy Marques, MD, MSc, of Leiden University in the Netherlands, and colleagues. “However, diagnostic uncertainty persisted in up to 30% of the cases after 2 years: 25% received a most likely diagnosis and 5% a possible diagnosis.”
At baseline, HLA-B27 positivity was found in 81% with a definite axSpA diagnosis and in 12% with a definite non-axSpA diagnosis. A family history of SpA was present in 48% and 32%, respectively; anterior uveitis occurred in 13% and 3%, and sacroiliitis or structural damage on MRI was seen in 67% and 4%.
“A single feature with sufficient accuracy to diagnose axSpA does not exist, but HLA-B27 positivity and sacroiliitis on imaging discriminate best between the axSpA and non-axSpA patients,” Marques and co-authors noted.
How Delays Can Be Reduced
To reduce diagnostic delay, widespread implementation of education, training, and simple referral strategies or prompts in primary care and in specialties treating extra-musculoskeletal manifestations (EMMs) are recommended, Sengupta and co-authors noted.
Rheumatology services should work directly with local service providers in primary and secondary care – including orthopedics, ophthalmology, gastroenterology, dermatology, and radiology — to establish clear referral criteria and pathways for suspected axSpA, they suggested.
“Knowledge of axSpA EMMs is continually advancing, and specialists should remain up to date with the latest research,” Sengupta and colleagues added. For example, within dermatology, hidradenitis suppurativa has been newly associated with axSpA as a possible EMM, they pointed out.
Disclosures
Husni reported relationships with Novartis, Eli Lilly, Janssen, UCB, AbbVie, and Pfizer.
Please enable JavaScript to view the