As a medical intern in the late 1980s, I’d occasionally see priests and rabbis on hospital wards, but we basically ignored one another. When we doctors walked into a patient’s room, they’d quickly leave, and when we exited, they’d enter. They seemed to operate in a wholly different realm. After all, we were scientific. They weren’t.
But in recent years, as patients’ and their families’ religious, spiritual, and existential attitudes and needs have shifted, so, too, have chaplains. Our nation’s religious landscape is changing, affected by, and affecting, broader political and religious polarization. In recent decades, self-identified Christians dropped by about a third. In the past 15 years, the number of religiously unaffiliated Americans has almost doubled.
advertisement
As a physician, I wanted to understand what these transformations mean for patients and their families, especially those facing serious disease, death, and dying. Hospital chaplains, I soon realized, address these challenges most, and I therefore set out to study them, speaking with 38 around the country and conducting a formal in-depth study of 23. What I learned continually amazed me.
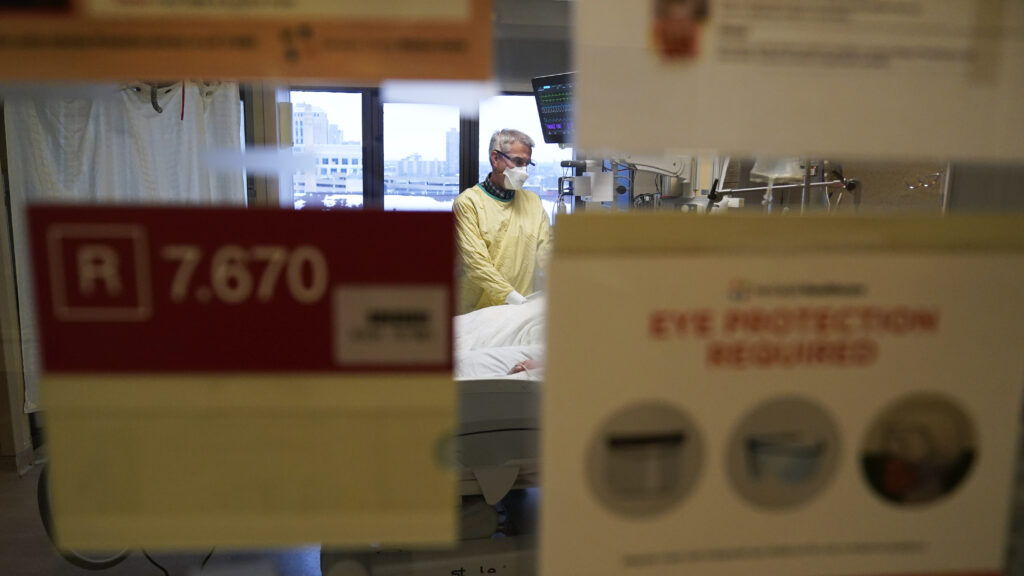
Amid new technologies, waning religions, shifting beliefs, fracturing health care systems, aging populations, and post-Covid health care worker burnout, chaplains are more important than ever. But they are often unappreciated.
Death terrifies most of us. We deny it until serious disease shatters our psychological defenses. Even religiously unaffiliated patients commonly struggle with “Why me?” and “What does my life mean?” and/or feel guilt over past actions. People seek connections to something beyond themselves that will continue on after death — through spirituality, children, nature, creative work — or they escape through the classic drugs, sex, and rock and roll. Increasingly, those facing their own mortality also grapple with decisions about whether to start or stop new medical treatments that extend the quantity, but frequently not the quality of life — whether to allow doctors to “play God.”
advertisement
In recent years, chaplains have evolved and often now see themselves as constituting a “post-religious” profession, taking nondenominational, multifaith, and humanistic approaches, and commonly receiving training in counseling. They aid patients, from evangelical to agnostic, atheist, and “nothing in particular,” in resetting priorities and finding sources of connection, meaning, purpose, and hope. Strongly committed to aiding vulnerable and underserved populations, chaplains remind doctors to uphold the dignity of every patient. Frequently, chaplains are the only hospital employees who have the time to talk with patients and families at length to understand patients’ experiences and perspectives in ways that doctors miss, gaining trust and discovering critical information.
At times, patients and families clash with medical staff regarding needs for more or less aggressive treatment, and chaplains serve as mediators. One chaplain I spoke with, for example, told me about an elderly patient with advanced, untreatable cancer and dementia. Doctors wanted to write a do not resuscitate order, but the patient’s daughter kept objecting, causing tense conflict. Finally, the chaplain spoke with this daughter, who didn’t want her mother “to die next week, on my birthday. She always seems to get sick right before my birthday.” The physicians consequently better understood the daughter’s position and waited.
Chaplains also help medical staff struggling with mounting moral distress and burnout due to spending less time with each patient, and more hours typing data onto computers.
Yet hospitals and doctors tend to marginalize, undervalue, and underfund chaplains, 62% of whom feel left out of medical team discussions, according to one study. Around 25% of hospitals lack chaplains altogether.
Unfortunately, chaplains’ functions are not readily quantifiable. Research on these professionals has begun but remains limited. Studies have attempted, for instance, to prove that patients’ and families’ satisfaction with hospitalization is higher if they saw a chaplain. But the results have been mixed, since sicker patients may be more likely to see chaplains but also to die, lowering overall satisfaction with hospitalization.
advertisement
Examination of the stories and details of chaplains’ actual experiences, however, tells a different tale. One chaplain, for instance, described a 94-year-old unresponsive patient on full life support. The family battled with the doctor, wanting more aggressive treatment because they were “praying for a miracle.” The chaplain told them, “We’re getting in the way of what God’s plan here may be.” Through compassionate discussion with the chaplain, the family eventually accepted the inevitable.
Another chaplain helped a 13-year old boy with cancer whose mother travelled around the country seeking a cure. She couldn’t face that he might die. She couldn’t even talk about it. When the doctors asked the chaplain to meet with her, a chaplain told me, this mother literally “put her fingers in her ears and said, ‘La-la-la-la-la. I can’t hear you! … I don’t want to talk about this!’ ”
After long discussions with the chaplain, the mother was eventually able to say to her son, “I’m concerned that the treatment isn’t working.” That comment gave the boy an opening to say, “OK. So, Mommy, when I die, I don’t want flowers because they’re for girls. I want stuffed animals. Then, after the funeral, bring them all to the hospital to give to all the kids.” He had it all planned out, but could never talk about it because she wouldn’t let him. He could see she couldn’t handle it.
One day, he told her that he had seen angels in his room, which distressed her. Yet the chaplain worked with her. The mother “finally said to him, ‘When you talk about angels, it makes me sad, because I think it means you’re not going to be here much longer.’ But he said, ‘No, Mom. The angels are here to help me. When it’s my time to go, Jesus will come for me!’”
Social workers could potentially address some of these issues, but their work often does not allow it, as they must usually focus on hospital discharge planning, finding nursing home beds, and applying for insurance. Mental health professionals rarely see hospitalized patients and families.
advertisement
A critical way to help our impaired health care system is therefore to encourage and use chaplains more. Hospital administrators, doctors, nurses, and other staff should recognize and further support chaplains, who can aid countless patients and families, even if in ways that statistics don’t fully capture.
When the boy with cancer died, his mother filled the funeral with stuffed animals, not flowers, and then hired a U-Haul and distributed them to her son’s fellow patients throughout the ward. She then called and thanked the chaplain.
Robert Klitzman is a professor of psychiatry in the Vagelos College of Physicians & Surgeons and the Joseph Mailman School of Public Health at Columbia University as well as the director of the in-person and online masters and certificate programs in bioethics. He is also the author of “Doctor, Will You Pray for Me?: Medicine, Chaplains and Healing the Whole Person.”