Glatter is an assistant professor of emergency medicine. Papadakos is a director of critical care medicine and a professor of anesthesiology, surgery, neurology, neurosurgery, and internal medicine.
Since the modern practice of anesthesia has evolved, providers have been concerned about pulmonary aspiration — when gastric contents enter the lung, resulting in severe complications including pneumonitis, and aspiration pneumonia, resulting in hypoxia, and potentially leading to excessive morbidity or death.
Since the inception of general anesthesia, healthcare providers have adhered to strict fasting rules: nothing by mouth after midnight. However, over the last decade, there has been a paradigm shift allowing clear liquids up to 2 hours prior to surgery for a procedure requiring anesthesia or sedation. In 2023, the American Society of Anesthesiologists (ASA) updated and liberalized its standards to allow healthy adults to drink carbohydrate-containing clear liquids up to 2 hours before elective procedures with general anesthesia, regional anesthesia, or procedural sedation.
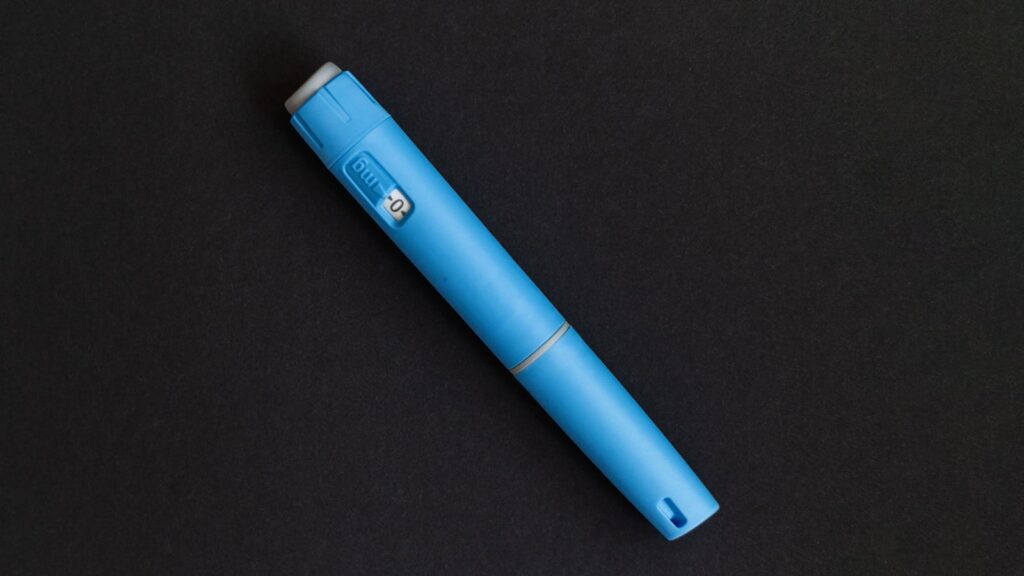
Even more recently, the ASA addressed the issue of glucagon-like-peptide-1 (GLP-1) receptor agonists before procedures that may require anesthesia or sedation. While originally prescribed for the treatment of type 2 diabetes, several drugs in this class of medications are now approved for weight loss. As a result, use of these game-changing drugs has exploded. Estimates suggest that approximately 12% of the U.S. population has already tried these drugs — the equivalent of one in eight people. This class of medications modulates the receptors that help us feel full and delays stomach emptying, which leads to the reduction of caloric intake and results in weight loss.
When the first GLP-1 drugs were introduced, many providers of anesthesia and sedation were very concerned about this aspect of delayed gastric emptying. The concern was based on classic teaching that a full stomach could lead to vomiting and thus stomach contents going into the lungs, leading to severe complications or death.
It became almost routine for providers and facilities to recommend discontinuation of these drugs for varied periods of time before a procedure. Initially, 2023 guidelines from ASA advised a 1-week and 1-day hold of injectable and oral GLP-1 agents, respectively, prior to surgery.
Updated guidelines were released last month by the American Society of Anesthesiologists, American Gastroenterological Association, American Society for Metabolic and Bariatric Surgery, International Society of Perioperative Care of Patients with Obesity, and the Society of Gastrointestinal and Endoscopic Surgeons.
The new guidance balances the concerns of delayed stomach-emptying with the potential risks of discontinuation of a medication, which can lead to elevated blood sugar levels in patients with diabetes that could also cause major issues during surgery and procedures. At its core, the goal has been to ensure safety for patients having surgery and other procedures without removing the benefits of GLP-1 drugs any longer than necessary.
The guidance noted that providers can minimize the risk of delayed stomach-emptying by having the patient follow a liquid-only diet for 24 hours prior to a scheduled elective surgery or procedure. For patients at higher risk of aspiration, an additional recommendation is that a point-of-care evaluation of the stomach contents be made using ultrasound prior to moving forward on the day of the procedure or surgery and modify their care as needed. This recommendation should lead providers to receive training in abdominal ultrasound.
The guidance also recommended that patients judged to be at elevated risk for delayed stomach-emptying need a detailed review on their use of GLP-1 drugs. This is especially important for patients in the early phase of treatment with GLP-1 medications, since they are at higher risk of aspiration. There is an escalation phase when the patients are taking increased doses of the drug — it typically lasts 4-8 weeks depending on which drug is being used and its clinical indication. In this subset of patients, elective surgery or the procedure should be deferred to a point after the escalation phase has passed and no gastrointestinal symptoms effects are noted by the patient.
Of course, patients having symptoms such as nausea, vomiting, abdominal pain, shortness of breath, or constipation should have surgery delayed until the symptoms resolve. This clearly reinforces the concept that all patients on GLP-1 medications need a detailed evaluation and open communication with their providers clearly explaining the risks and benefits associated with GLP-1s and preoperative planning.
The guidance did not specifically address a common airway management device used in many procedures known as the laryngeal mask airway (LMA). Special caution may be required in caring for patients who are currently prescribed GLP-1 drugs and require placement of an LMA. This guidance will continue to evolve as more data from patient encounters evolve.
While the current guidance is not evidence-based (some studies suggest low aspiration risk with GLP-1 use, while others come to the opposite conclusion), it is more nuanced and reflects shared decision-making. It balances safety with the therapeutic advantages of these drugs and the need for continuation of surgical and procedural care in this ever-growing patient population using GLP-1 drugs. But ultimately, it falls to individual providers to make clinical judgements suited to the risk profile of each patient undergoing a procedure. Decision making in this regard must take into account both aspiration risk and the risks of discontinuing GLP-1s (hyperglycemia, hydration status) for up to a week prior to a scheduled surgery or procedure.
There should be ongoing monitoring of the effects of GLP-1 medications in patients undergoing surgery and other invasive procedures to rapidly identify any ongoing safety issues. If necessary, the guidelines should be modified to provide for maximal patient safety.
Robert Glatter, MD, is an assistant professor of emergency medicine at the Zucker School of Medicine at Hofstra/Northwell, Lenox Hill Hospital, and Northwell Health in New York. Peter Papadakos, MD, is director of critical care medicine and a professor of anesthesiology, surgery, neurology, and neurosurgery at the University of Rochester in New York. He is also a professor of internal medicine at the Mercer University School of Medicine in Macon, Georgia.
Please enable JavaScript to view the