- Over 4.7 years of follow-up, no link emerged between antibiotic use and dementia risk in healthy older adults.
- However, the findings may not apply to the general older population.
- Earlier evidence about the relationship between antibiotic use and cognition has been mixed.
Antibiotic use didn’t raise the risk of dementia in healthy older adults, a prospective study suggested.
Over about 5 years of follow-up, antibiotic use was not tied to higher dementia incidence (HR 1.03, 95% CI 0.84-1.25) compared with no antibiotic use, according to Andrew Chan, MD, MPH, of Harvard Medical School in Boston, and co-authors.
It also wasn’t linked with cognitive impairment with no dementia (HR 1.02, 95% CI 0.94-1.11) or to subsequent declines in cognitive scores, the researchers reported in Neurology.
The findings were based on observational data for 13,500 people ages 70 and older who had participated in the ASPREE trial of aspirin, as well as its extension.
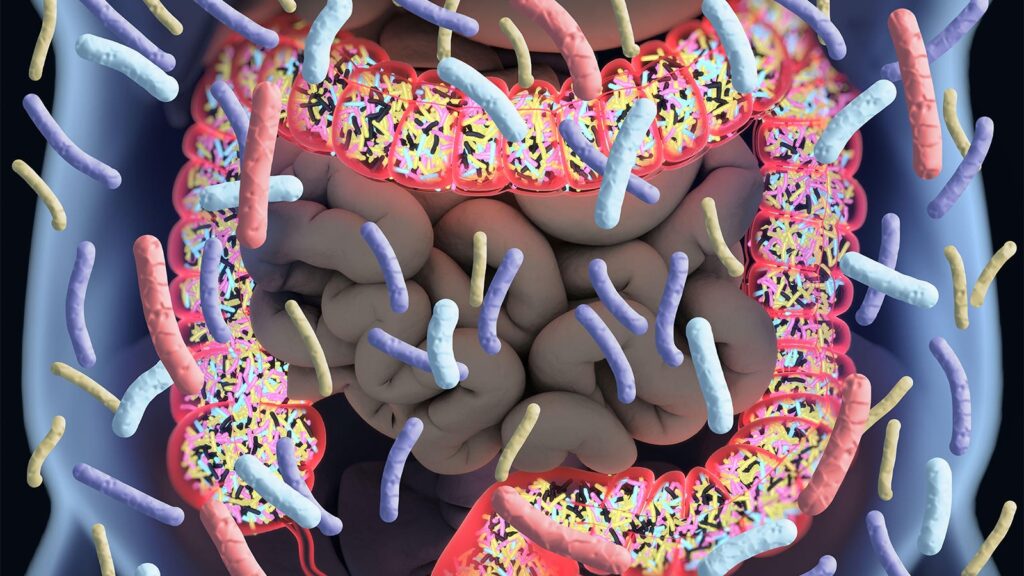
Antibiotics can disrupt the microbiome, Chan noted. “Because the gut microbiome has been found to be important for maintaining overall health, and possibly cognitive function, there was concern that antibiotics may have a harmful long-term effect on the brain,” he said in a statement.
“Given that older adults are more frequently prescribed antibiotics and are also at higher risk for cognitive decline, these findings offer reassurance about using these medications,” Chan added.
That reassurance comes with caveats, said Wenjie Cai, MD, and Alden Gross, PhD, of Johns Hopkins University Bloomberg School of Public Health in Baltimore.
ASPREE recruited people from Australia and the U.S. who had no serious disability, cardiovascular events, dementia, or serious intercurrent illness, Cai and Gross noted in an accompanying editorial.
“Readers should be cautious when interpreting and implementing these findings to inform rigorous clinical practice,” the editorialists pointed out. “This study offers insights for clinicians and healthcare providers working with healthy older adults who share similar health profiles with those in this study.”
Earlier evidence has been mixed about the relationship between antibiotic use and cognition. In the Nurses’ Health Study II, women with at least 2 months of antibiotic exposure in midlife had lower mean cognitive scores 7 years later. An early randomized trial showed that daily oral antibiotic treatment for 3 months attenuated cognitive decline in people with Alzheimer’s disease, but a larger follow-up trial showed different results.
Chan and colleagues evaluated antibiotic prescription data and cognitive test results from 13,571 ASPREE participants. In 2018, the trial was extended as ASPREE-XT, an observational study. Mean age was 75 years, 54.3% of participants were female, and 98.6% were white.
Cognitive tests were conducted at baseline, 1 year, then every 2 years. The tests assessed global cognition, episodic memory, language, executive function, and psychomotor speed.
Antibiotic data were based on filled prescription records. Overall, 62.5% of participants used any antibiotics at least once between trial enrollment and the second follow-up visit.
During a median of 4.7 years after the second follow-up visit, 461 incident cases of dementia and 2,576 incident cases of cognitive impairment with no dementia were reported.
Higher frequency of antibiotic use was not associated with dementia or cognitive impairment; neither was long-term use. No relationship with dementia or cognitive impairment emerged in analyses by antibiotic class, even in drug classes like fluoroquinolones or metronidazole that could reach higher concentrations in the central nervous system.
The study has several limitations, Chan and colleagues said. Antibiotic information was based on filled prescriptions, which may not reflect actual use. The healthy nature of participants at baseline means the findings may not be generalizable to the general older population. Residual and unmeasured confounding also may have influenced results.
In addition, “the relatively short duration of study follow-up may not be able to capture the long-term effects of antibiotic use on cognitive aging,” the researchers acknowledged.
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
The ASPREE trial and ASPREE-XT were supported by grants from the National Institute on Aging and the National Cancer Institute at the NIH, and by grants from the National Health and Medical Research Council of Australia, and by Monash University and the Victorian Cancer Agency.
Chan reported relationships with Pfizer, Boehringer Ingelheim, Bayer, and Zoe Ltd. One co-author disclosed a relationship with Merck.
Cai and Gross had no disclosures.
Primary Source
Neurology
Source Reference: Wang Y, et al “Antibiotic use and subsequent cognitive decline and dementia risk in healthy older adults” Neurology 2024; DOI: 10.1212/WNL.0000000000210129.
Secondary Source
Neurology
Source Reference: Cai W, Gross A “Are antibiotics associated with cognitive decline? Not for healthy older adults” Neurology 2024; DOI: 10.1212/WNL.0000000000210255.
Please enable JavaScript to view the