In recent years, low-level electrical stimulation has emerged as an effective rehabilitative tool for people with spinal cord injuries. But not all patients have benefited because researchers often exclude people from studies if they have involuntary muscle spasms, known as spasticity.
In a new study in Science Translational Medicine, researchers in Europe say they have developed a new type of electrical stimulation therapy that addresses spasticity while delivering comparable rehabilitative results. While the pilot study’s sample size is small — only two participants — their quality of life improvements were significant.
advertisement
“We are just starting to understand how to modulate the activity of the spinal cord. This is not the end of the story. We are showing that you can unlock properties of spinal cord neuromodulation for doing more,” said Silvestro Micera, a neuroengineer at the Swiss Federal Institute of Technology in Lausanne, Switzerland. “The technology that we are using right now, we are going to combine with other technology like Lego bricks.”
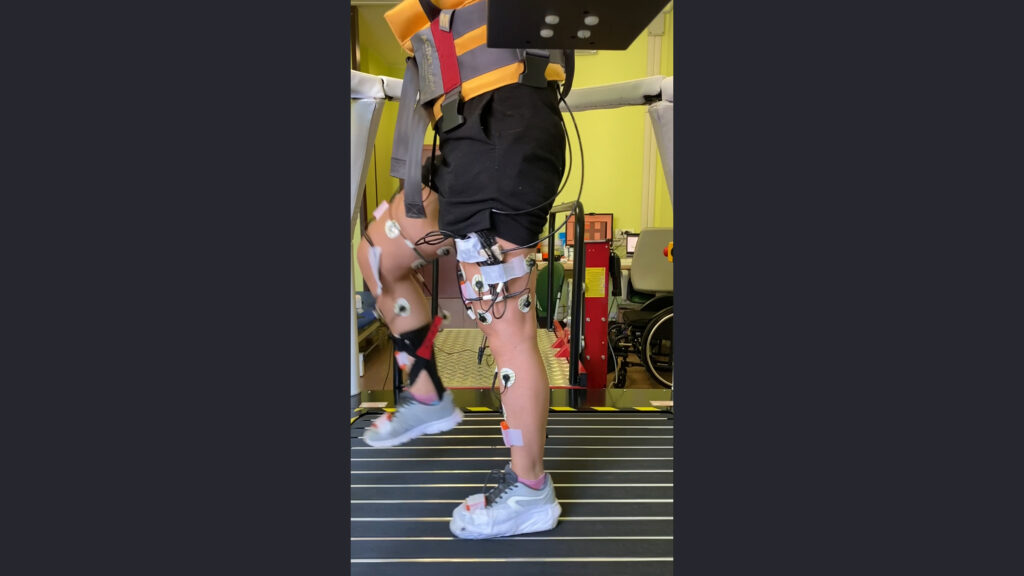
Traditional epidural electrical stimulation strengthens the contraction of the muscles and can improve the muscle’s functioning. But when a person has spastic muscles, the clinicians need to reduce, not enhance, the contractions. Micera and his colleagues found that high-frequency stimulations, in addition to more traditional low-frequency electrical zaps from a machine used for treatment of chronic pain, held the spasticity at bay while still improving the participants’ ability to walk.
Experts debate spasticity’s prevalence among those with spinal cord injuries, but potentially as many as 67% of people with spinal cord injuries may experience it. The contractions are often painful and leave the muscles stiff, and medications to address spasticity are tough on the kidney and can lead to further weakness. Finding a way to help this population could further aid people with conditions such as paraplegia, stroke and Parkinson’s disease. The new study is the latest sign that electrical stimulation is a potentially effective tool for clinicians to treat injuries up and down the spinal cord.
advertisement
STAT spoke with Micera and two of the paper’s other authors to better learn how their tweak to electrical stimulation can help people with spasticity. Simone Romeni is a doctoral candidate in Translational Neural Engineering at Swiss Federal Technology Institute of Lausanne, and Pietro Mortini is a neurosurgeon and professor at Università Vita-Salute San Raffaele in Milan.
This interview has been edited for clarity and length.
Why did you decide to tackle this problem of spasticity in spinal cord injuries?
Silvestro Micera: A large fraction of patients who could benefit from electrical stimulation have spasticity, so abnormal contractions and spasms due to the spinal cord injury. It was not possible with the standard spinal cord stimulation to help these patients. The idea was to find a way to take two pigeons with a stone: to restore locomotion and at the same time also reduce the spastic symptoms. Because if you are able to remove the spasticity, the patient can get more rehabilitation and walk better.
Pietro Mortini: If you have a partial spinal cord injury, that means you have a residual motor function that makes it difficult to walk. Spasticity blocks this very limited ability to walk. So if you use our technology with high frequency electrical stimulation, you have the ability to remove the spasticity.
Simone Romeni: Spasticity is not a lesion, it’s not something that you can just image and then see and is simple to measure. It’s something that you need to go and look for, you need to do functional tests and manipulations. You find it when the therapist tries to passively mobilize the limbs of the patients, they find some resistance that shouldn’t be there. In a healthy person, if you try to close the knee, to flex the knee of the subject, you feel no resistance. In these patients, if you do it at a certain speed, you will see that the muscle opposes this motion.
How does spasticity work? Why are these muscles contracting?
Romeni: Spasticity is an umbrella term to denote a lot of different phenomena that are linked to this hyperactivity of the spinal cord that gives these unwanted contractions. When there is a nerve signal that comes from the periphery, it is amplified in the spinal cord because of a lesion, which can overreact. If we block the thing that is coming from the periphery, and we don’t have it reach the spinal cord, the spinal cord will not overreact and the muscles will not become spastic and stiffen.
advertisement
High frequency stimulation basically blocks nerve transmission in a temporary and completely reversible way. So we switch on the stimulation, the high frequency stimulation, and the signals from the periphery, they don’t get to the spinal cord, and the spinal cord has nothing to react to, and we have solved spasticity.
Why wouldn’t this interfere with other signals coming to the spinal cord, namely the brain?
Romeni: The spinal cord has two flows of information, a flow from the periphery and a flow from the brain. These patients have an incomplete lesion, so they have partial control over their limbs. What we have measured is that the control that they have on the muscles, what comes from the brain, that flow is not blocked. If they want to stand up, they can stand up.
The one that is responsible for the spasticity is the one coming from the periphery. So we just block that one for certain muscles, which means that the patients can still walk. Then we are using traditional low-frequency electrical stimulation on the muscles that are weaker, so that we have the best of the two worlds.
It’s like we are jamming up a telephone line. My guess is that we are not completely blocking that way. We are just really, really, really reducing it so that there are not these hyper reactions, so we are almost blocking it, but not completely.
Should we be worried about blocking nerve signals?
Romeni: We still don’t have very reliable means of investigating signals inside of the spinal cord. So it is very, very difficult to get a conclusive answer of exactly what is happening. The fact that this is safe, we are pretty sure. There were no side effects in our study. This technique of jamming the transmission of peripheral nerve signals is something that is known — We didn’t know that it could be used somehow on the spinal cord to block spastic muscle hyper activation.
How did the patients fare after receiving the high frequency stimulation?
Micera: The first patient has been able to walk quite normally for quite some time, though they had a milder disability compared to the second. Both of them significantly improved their performance and ability in walking. All the clinical scales in walking for 6 min, the endurance of walking, all of these things in both patients significantly improved. It’s only an n=2, but in both of them it worked pretty well, there was a significant improvement in their locomotion activities. Of course we are not restoring the full ability of walking, but we are giving patients the possibility to walk for minutes, for hundreds of meters in a way that they can’t now. It would mean a significant improvement in the quality of life.
advertisement
Mortini: The timing for implanting the patient is key. In our two patients, the second patient had a spinal cord injury five years before our operation — the volume of muscles, the tone of the muscle can decrease over time. In the future, it would be better to operate on the patient after a very short time after the injury. We are in a condition where we include the patient only after one year, so that’s a regulation for spinal cord injury research. Our idea is to include patients a very short time after injury, maybe a couple of months.
How do you think the technology will go when scaled up?
Micera: That’s what we are planning in the near future, bringing it to more patients. We have now the first 10 patients that Professor Mortini is recruiting. It’s honestly difficult to say whether it’s going to work with all of them right now. We are confident we are able to apply this in a smart way for all the patients with spasticity. But it’s too early to really say.
The personalization of when, where, and how to activate the high frequency is going to be one of the issues. We used different timing and different methods of high frequency stimulation for the two patients, because each patient is different. I think that’s one of the next challenges for us. Each lesion, if it is an incomplete lesion, each lesion is pretty different. This means that each patient will have different residual skills, different levels of plasticity in different levels of muscles. They are simply different.
This is the first paper of at least 15 years of collaboration between our teams, and the idea is to combine technologies to treat patients with many different kinds of conditions. These patients have a significant reduction in quality of life. Helping them, it’s very important, clinically.
Are you planning to develop a rubric that clinicians who use electrical stimulation therapy can follow? How will they know how to use this new technique?
Romeni: There are two ways that I think they can be quite useful. We are working quite a lot on computational models, including an MRI that characterizes the electrical response of muscles to stimulation. That can allow us to replicate the spasticity patterns that a patient exhibits, especially since every patient is different. We need to understand exactly what our windows of operation are.
advertisement
The other side is the biomechanical part. We need to understand what is the impairment that spasticity provides to the patient, and at which point, during the rehabilitation workflow, it will become important.
Micera: In order to find when to use high frequency stimulation for which kind of muscles, what we need to have is a digital twin of the person. We would be able to replicate, to simulate what we can do with the patient in order to understand a bit better when we can.
How does this bode for the future of neuromodulation?
Micera: We realized using high frequency works and it can help. But what is clear is that we can do more. It’s not my protocol against your protocol. It’s, find different tools that we can use together for different patients in different times of rehabilitation. And we have now with high frequency stimulation a new tool, but very likely we will find, or others will find in the future, additional tools. Different technologies can be used for other situations, for stroke, for multiple sclerosis. Other people are starting to use it for Parkinson’s. Neuromodulation for different tools for different parts of the nervous system can be used for many kinds of neurological problems. It’s a small niche, but with a lot of need for clinical and technological help.
Mortini: At least for Europe, where we have a public health system. They have a tremendous high social cost. If you are unable to move, you are sitting in a wheelchair. You need the architectural changes in your house, your building. You need a new car. You are unable to walk in a street, because in Europe, for example, there are many, many streets that are ancient, so you are unable to move everywhere. You can walk with our technology. So it’s very important from a social point of view.