In November 2022, Dennis Selkoe, a Harvard professor of neurologic diseases and among the most celebrated and prolific Alzheimer’s researchers, chastised me over lunch.
I had just broken a story in Science about the horrific death of a volunteer in a trial of lecanemab, a much-anticipated new drug to treat Alzheimer’s by flushing certain dangerous substances from the brain. The woman suffered a massive cerebral hemorrhage. A pathologist said it was like “her brain exploded.”
advertisement
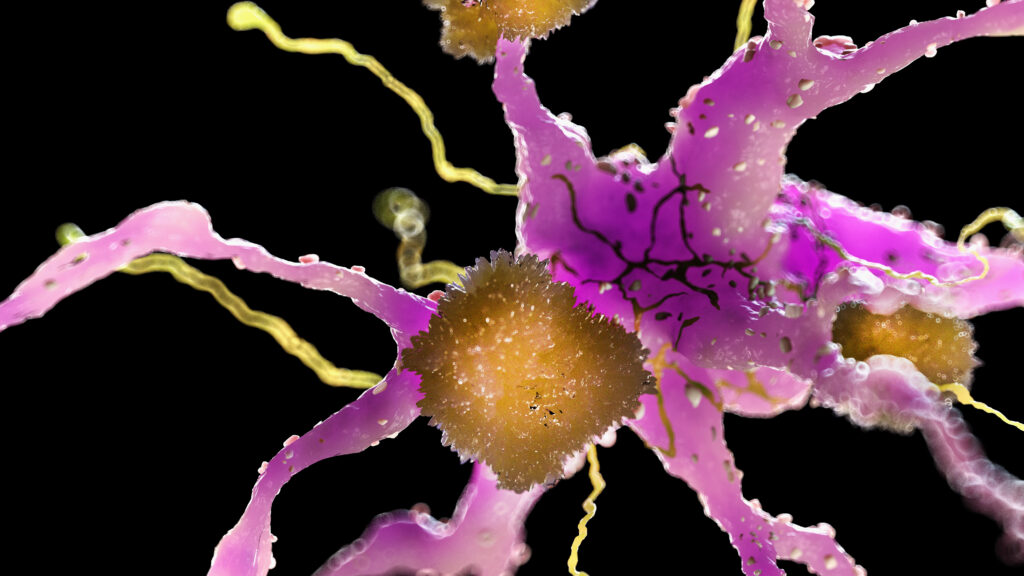
Leaning over a plate of pasta during lunch at an upscale San Francisco hotel, Selkoe pressed me to concede that some in the media are far too pessimistic about such drugs derived from the “amyloid hypothesis,” which blames the build-up in the brain of “amyloid-beta proteins” — including the sticky plaques thought to promote a cascade of biochemical changes that lead to Alzheimer’s dementia. We owe greater deference, he said, to doctors “who have taken care of hundreds of patients with Alzheimer’s and have been through this long journey.”
Selkoe was shrewd. I was skeptical about lecanemab, which in testing only minutely slowed cognitive decline among some patients with mild Alzheimer’s symptoms, costs tens of thousands of dollars per patient annually, and poses deadly risks. The drug’s benefit seemed so subtle as to be imperceptible to doctors, patients, and caregivers. But he implied that only misguided contrarians could dispute that lecanemab established the amyloid hypothesis as fact, and that such drugs would illuminate the path to solve the Alzheimer’s puzzle.
That notion of consensus struck me as absurd, as did his description of the media coverage, which often tilts to fawning approval of any treatment that offers a glimmer of hope, however dim. But Selkoe insisted that this was “objective evidence” that reducing amyloid in the human brain produces better cognitive outcomes. “I’m on the right side of history,” he said.
advertisement
Lecanemab, described by credible neuroscientists as “disease modifying” — affecting the putative cause of the illness rather than temporarily reducing symptoms — supposedly slows cognitive decline by flushing many amyloids from the brain.
The scientific conference that had brought us to San Francisco became a lecanemab lovefest — a victory lap for Selkoe and his allies. It was heralded as a breakthrough despite meager benefits and some ghastly fatalities and brain injuries among trial volunteers.
Not entirely reductive in his thinking, during our discussions the following year Selkoe conceded that the amyloid hypothesis couldn’t fully explain Alzheimer’s disease. Viral infections, for example, might “contribute in some way” to the cascade of pathology that amyloid proteins cause. Nonetheless, his role in strong-arming the field to favor a focus on amyloids above all else — “the scientific equivalent of the Ptolemaic model of the Solar System,” in which the Sun and planets revolve around Earth, as one scientist called it — seems beyond debate. He’s a key member of what some have described as a “cabal” or “mafia” whose influence, prestige, networking, and prolific writings help enforce a singular scientific and commercial vision.
Others went so far as to suggested a moniker even more likely to rankle seemingly committed rationalists: a “Church of the Holy Amyloid,” with Selkoe among its high priests.
Farmers rotate crops to enrich the soil. Skeptics argue that the amyloid mafia fostered the equivalent of a scientific monoculture that depleted the research landscape.
Scientific hegemony
The amyloid mafia is not a real organization, of course. But it aptly characterizes power figures who some say steer grants and career opportunities away from those who suggest alternatives. “It became gradually an infallible belief system,” Zaven Khachaturian, former director of Alzheimer’s research at the National Institute on Aging (NIA), part of the National Institutes of Health, told journalist Maja Beckstrom in 2019. “Everybody felt obligated to pay homage to the idea without questioning. And that’s not very healthy for science when scientists … accept an idea as infallible.”
advertisement
That influence seemed apparent in the years that followed a famous 2006 experiment in Nature that tied cognitive decline to a specific protein dubbed amyloid-beta*56. That amyloid subtype was described as a “toxic oligomer” — soluble in the fluid that bathes the brain, unlike the sticky plaques commonly associated with Alzheimer’s. The study became central to the evolving hypothesis. Selkoe often cited the 2006 study and saw his own oligomer ideas ascend.
In 2022 my article in Science exposed apparently doctored scientific images at the heart of that paper — a copy-paste job that falsely showed the presence of proteins that supported the research premise — which was retracted in 2024. But oligomer funding from NIH had skyrocketed from near zero in 2006 to more than $333 million in 2021 alone. Since 2002, the majority of major human trials testing Alzheimer’s drugs have focused on how to remove amyloids from the brain — including most large drug studies that can cost hundreds of millions of dollars. Such spending exasperates skeptics who say it crowds out other ideas to the detriment of patients.
“You can’t look at brain tissue and believe beta amyloid has nothing to do with it. It’s absolutely everywhere. But we’ve got lots and lots of patients who have tons of amyloid … with normal cognition,” said Matthew Schrag, a Vanderbilt University neuroscientist who discovered the doctored images in the 2006 Nature paper while working independently of his employer. “Biology is trying to tell you that there’s clearly more to the story.”
University of Cincinnati neuroscientist Alberto Espay found that among 51 anti-amyloid trials conducted from 2002 to 2022, 80% had successfully reduced amyloid-beta deposits. But the treatments had outperformed the placebo only in the dubious case of the drug Aduhelm — the dangerous and ineffective predecessor to lecanemab that was pulled off the market.
In 2022 lecanemab — the next great hope — neared the end of clinical trials. Preliminary results suggested minimal effectiveness. Then a confidential source reached out to me about a horrific death in the trial. A 65-year-old woman who received lecanemab infusions entered Northwestern University Medical Center in Chicago with an apparent blood-clot-induced stroke. She was given a common, often-lifesaving intervention, the clot-busting medicine tissue plasminogen activator (tPA). Bleeding throughout her brain’s outer layer instantly followed.
advertisement
“As soon as they put it in her, it was like her body was on fire,” the woman’s husband later told me. “She was screaming, and it took, like, eight people to hold her down. It was horrific.” Soon, a priest came to deliver the “Anointing of the Sick” prayer. The woman suffered seizures and was placed on a ventilator. After a few days the family approved disconnecting the device, and she died. Her doctors had never seen a case of similarly massive bleeding.
My report in Science on the death quickly became the subject of global headlines: The most promising anti-amyloid treatment was also a killer. Less than a month later, a new source came forward to tell me that her mother, another lecanemab trial participant, died after hideous brain swelling and bleeding, and violent seizures.
As lecanemab swept amyloid plaques from participants’ brains, it often induced brain bleeding or swelling. Dozens endured painful symptoms, and at least five died or suffered serious brain injuries. No one knows whether such symptoms cause long-term damage.
Lecanemab also shrinks the brain more rapidly than Alzheimer’s itself. Scientists have no clear idea what that means over the long run — and it will be impossible to find out from the key study of the drug. That’s because the drug’s maker said it would keep the data secret. No independent experts can examine the details on what happened to patients’ brains or follow what happens to them in years to come.
Lecanemab offered the amyloid hypothesis as the one true path to relieving the misery of millions. That promise has never decreased symptoms for a single patient, let alone cured anyone. So, to many doctors, it looked like a cruel charade.
Yet the FDA provisionally approved lecanemab (brand-named Leqembi) even before seeing the major trial results. In July 2023, it delivered full approval. FDA ignored requests for a program that would have required educating patients and doctors, and monitoring outcomes to contain risks such as deadly brain bleeds.
advertisement
Critics objected that the amyloid lobby — pharma companies and the patient advocacy groups, famous doctors, and researchers they underwrite — had gone too far. Advocates of Leqembi countered that individuals with a harrowing disease and their loved ones should be able to judge the risks and benefits. In any case, scientists agree that carefully screened trial participants face lower risks. Deaths and brain damage will almost certainly rise sharply if tens of thousands of patients demand Leqembi from average doctors all over the country.
That worry led the FDA to require a “black box warning” to the lecanemab product label. A black box denotes risk of death. Every doctor who prescribes it has to ask a sobering question: Am I prepared to face the moral, legal, and financial liability if my patient suffers brain damage or dies from this drug? By early 2024, only 2,000 patients had been treated with Leqembi — fewer than the number that participated in clinical trials.
The FDA waved through Eli Lilly’s look-alike drug Kisunla in 2024.
Lon Schneider, an Alzheimer’s researcher at the University of Southern California, studies amyloid vaccines and takes fees or grants from the top makers of anti-amyloid drugs. He’s hardly an amyloid hater. Schneider noted that most Alzheimer’s patients get the terrible diagnosis late in life. “So much of the amyloid world is built on an almost biblical end-of-times story,” he said in an interview. “But half of the people who get Alzheimer’s after age 82, frankly, don’t have that much of a problem with its slow progression. Many die with it, not from it,” a very different disease than the tragic, rare cases of younger people featured in the media.
“Lecanemab offers just a tiny effect after 18 months. But its advocates use dream statistics to project forward,” Schneider said. “‘We will see a bigger effect,’ they say. Then the message becomes ‘proof’ that people benefit for years, and many will be ‘survivors.’ The study wasn’t designed to show long-term outcomes. … But if you say it long enough, you will believe it.”
advertisement
Costly dream
When the FDA fully approved Leqembi, the U.S. Centers for Medicare and Medicaid Services approved payments. With pricing set at $26,000 annually, its makers, Eisai and Biogen, hope to earn more than $10 billion a year on the drug by 2031. Medicare will also cover costly brain scans for diagnosis and safety monitoring that could run the bill to as high as $90,000 per patient year, according to Schneider, and boost overall costs above payments for any other drug covered by Medicare. And many recipients would owe $6,600 in copays, a substantial portion of the $50,290 median annual household income for seniors, making Leqembi unaffordable for many who would ostensibly benefit from it. If widely adopted, it would almost certainly spike drug premiums for Medicare recipients.
He wishes the price were lower, Selkoe said, but if Leqembi works as described, it would offset Medicare spending on nursing care by keeping people in their own homes a bit longer. If so, most of those costs would be pushed to family caregivers, who would also pay for transportation and management of common side effects for regular infusions through a vein.
“Having actual therapies that even have a small beneficial effect is positive and great for patients,” said one skeptic, Stanford University neuroscientist and Nobel laureate Thomas Südhof. “I wouldn’t call it a breakthrough, though.”
To Südhof, rather than proving the amyloid hypothesis, Leqembi does the opposite. Because after removing amyloids, symptoms of dementia still steadily worsen. “I am not sure that the approval of the antibodies is actually a positive thing,” he said. “I worry that they might actually slow down the field by providing a commercial impediment to developing advances that might provide a bigger impact.”
I asked Selkoe if he foresees a day when better and better anti-amyloid drugs will go beyond minutely slowing the progression of Alzheimer’s. Will they improve cognition or even cure the disease? His downbeat answer surprised me: “I doubt it.”
advertisement
Medication for life
But another untested hypothesis holds that these or similar drugs might someday prevent Alzheimer’s: What if we treat healthy people? At age 55 or 60, such a drug might head off amyloid plaque deposits before they cause cognitive symptoms. Give them a drug for year or longer, maybe for decades, to monkey-wrench the amyloid device of destruction. It’s a drugmaker’s dream — the potential for millions of people to take a costly product for much of their lives. Eisai is underwriting just such a trial for lecanemab.
Another company has started a trial targeting amyloid deposits in patients as young as 18 who have or might have genetic markers associated with Alzheimer’s. Some scientists and clinicians challenged the ethics of administering such drugs to asymptomatic people based on the presence of biomarkers showing that they might someday develop Alzheimer’s.
“As we cannot conceive of any alternatives to the ‘amyloid is toxic’ idea,” Espay told me, “after this fails (which it will) we will move to a primary prevention trial targeting children.”
The term “preclinical Alzheimer’s” has come into play, affecting an estimated 315 million people globally. It was codified in a major study underwritten by Alzheimer’s drug makers Roche and Biogen. A 60-year-old who tests positive for those biomarkers, for example, faces a less than one in four lifetime risk of developing dementia — yet would be considered a candidate for drugs that can have lethal side effects. A younger market for anti-amyloid therapies understandably excites such companies — and infuriates skeptics.
“The amyloid hypothesis has a very simple story. We get rid of this evil thing, and things go back to normal. But that didn’t happen,” Journal of Alzheimer’s Disease editor George Perry said. “So now they say, ‘Patients won’t decline as fast. They will eventually get better. Maybe we’ll start treating earlier.’ How scary is that, when you start treating 50-year-olds with something that causes cerebral bleeding?”
advertisement
Selkoe said amyloid skeptics don’t understand the science. “They don’t feel it the way that I have felt [it] for 40 years,” he said. “It’s fine to bring up the specifics about price, danger, and degree of meaningful benefit. But we should put aside the notion that the science behind this hypothesis has not gelled, has not been sufficiently validated.” Flipping their script, he compared skeptics to Earth-worshipping Ptolemaic scholars. Yet when I asked if he ever had doubted the amyloid hypothesis, Selkoe said no. He conceded that “once you get into a line of thinking, I’m sure that for all of us, you’re stuck on that line.”
The late science journalist Sharon Begley, writing in STAT, described career-altering obstacles faced by some who bucked the hypothesis. One received whispered advice: At least pretend in research proposals that her work was linked to amyloids. Venture capitalists and major biopharma companies told others who tried to start companies that they would back only an anti-amyloid approach.
Ruth Itzhaki of the University of Manchester in England saw her 1991 alternative explanation — a link between the herpes virus and Alzheimer’s — rejected by top publication after top publication. Two decades later, a peer reviewer of a funding proposal she’d put together responded, “Very few [of your] papers have appeared in the most highly regarded journals.”
“I thought research should be judged on its own merits,” Itzhaki told me. She never rejected a role for amyloid. She only questioned whether it caused the disease.
Science is too vast for any idea to gain a total monopoly. But the amyloid hypothesis has retained its dominance from shapeshifting, Protean flexibility. “I hate the phrase, ‘the amyloid hypothesis,’” said Südhof, who sees amyloids within a complex interplay of contributors to Alzheimer’s. The general idea has been called the “amyloid plaque hypothesis,” the “amyloid-beta hypothesis,” the “amyloid cascade hypothesis,” and the “amyloid oligomer hypothesis,” he noted. Because it continually changes, Südhof added, “You can never disprove it.”
advertisement
Copyright © 2025 by Charles Piller. Adapted from the book “Doctored: Fraud, Arrogance, and Tragedy in the Quest to Cure Alzheimer’s” by Charles Piller published by One Signal Publishers, an Imprint of Simon & Schuster, Inc. Printed by permission.
Charles Piller is an investigative journalist for Science.