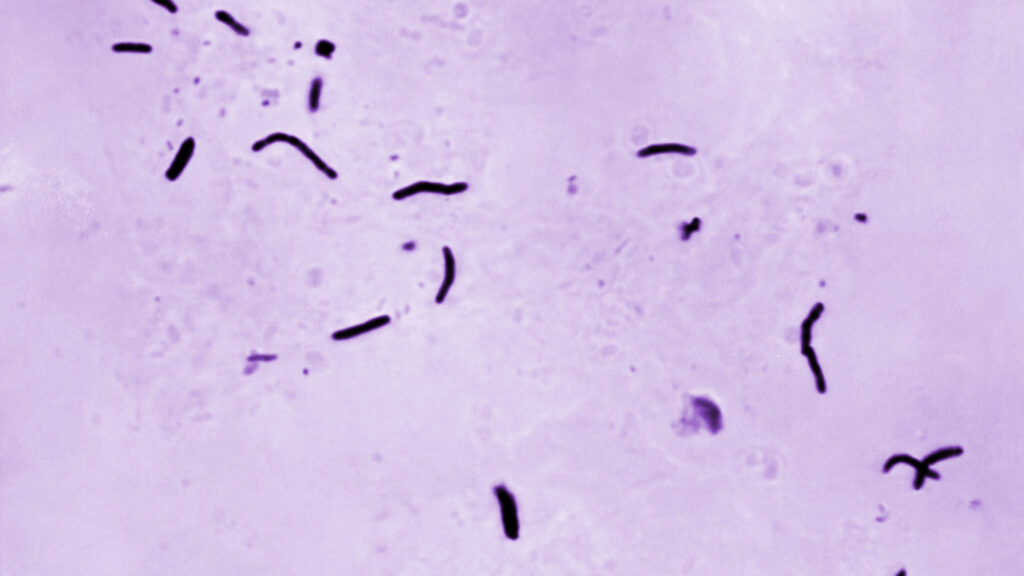
An ongoing tuberculosis outbreak in the Kansas City metropolitan area straddling Kansas and Missouri has made headlines across the country, a rare feat for an infectious disease too often ignored in the United States. While previous reports describing the outbreak as “the largest in U.S. history” were quickly debunked, it is one of the bigger TB outbreaks within a one-year period over the past several decades: Since January 2024 in Wyandotte and Johnson counties, there have been 67 cases of active TB (symptomatic disease that can spread by air and can be fatal if left untreated,) and 79 cases of TB infection (asymptomatic and non-infectious, but which can eventually turn into active disease.) Two deaths have been linked to the outbreak.
As longtime TB researchers and activists, we seldom see this much attention paid to TB in the United States, let alone in the Midwest, where all three of us grew up. While TB makes more than 10 million people sick each year, fewer than 10,000 of them are in the United States. But the outbreak in greater Kansas City offers a stark reminder of the importance of public funding for TB research and programming — and the potentially deadly stakes of the Trump administration’s assault on global and public health infrastructure.
advertisement
Even though TB is curable and preventable, it remains the world’s deadliest infectious disease, killing about 1.25 million people every year. TB mortality is largely due to lack of access to prevention, diagnosis, and treatment. Public investment makes the care and tools that fight TB available to everyone who needs them and saves lives. This includes funding the work of domestic local health departments: More than half the people living with active TB disease linked to the Kansas City-area outbreak have already been cured; the rest are still taking their course of curative treatment. The vast majority of people with TB infection in Kansas and Missouri have also taken TB preventive treatment (TPT), which will protect them from developing active disease. Local health departments traced close contacts of people diagnosed with TB and administered treatment and prevention free of charge. That not only benefits patients themselves, but also their neighbors. The Centers for Disease Control and Prevention TB Elimination Division enhances health departments’ capacity to stop domestic TB outbreaks in their tracks.
Just as everyone living in the greater Kansas City area and beyond benefits from TB programming through local health departments, we’re also all better off when public health officials have the best possible scientific tools to find, cure, and prevent TB. Since the Treatment Action Group added TB to its mission back in 2002, we’ve seen global TB advocacy help win major advancements in TB research and development. Just over 20 years ago, we were still using technologies from the 1800s to diagnose TB, and treating it with imperfect drugs discovered back in the 1950s and 1960s. It could take many weeks and several facility visits to even diagnose a case to begin with, people had to stick with arduous medication regimens for extended periods of time and deal with severe side effects, and barely anyone with TB infection underwent TPT because the preventive regimen was as long as treatment for active disease. In other words, the TB interventions we were stuck with were a bit like cutting steak with a butter knife — but with life-and-death consequences.
Today, regimens for TB prevention and treatment are shorter and less toxic than ever before. These strides are largely thanks to public investment in TB research and trials. For example, one clinical trial sponsored by the National Institutes of Health and the CDC showed that TB infection can be successfully treated with 12 weeks of a once-weekly treatment called 3HP — findings that allowed this shorter, gentler regimen to replace the previous nine-month regimen of 270 daily doses. A related CDC trial showed that this 3HP regimen is safe for young children, making TB prevention more accessible for kids. Yet another NIH and CDC trial demonstrated that treatment time for drug-susceptible TB can be cut from six months to four months. For drug-resistant TB, a TAG analysis found U.S. government investments in R&D for the drug bedaquiline exceeded spending by product developer Johnson & Johnson by several times, ultimately enabling DR-TB treatment to be shortened from 18 months or more to as little as six months.
advertisement
These discoveries would probably never have happened, and countless lives would have been unnecessarily cut short, without U.S. government spending.
The fact that health departments in Kansas and Missouri had access to these scientific breakthroughs makes TB outbreaks more manageable — stopping the outbreak well short of becoming U.S. history’s largest! — and makes getting sick with TB less traumatic and disruptive for people living with the disease, their families, and communities. Ensuring that everyone on Earth has access to the best available tools reduces the TB burden everywhere, ending chains of transmission as quickly as possible.
Make no mistake — we still need even better tools, including a broadly effective vaccine, to end TB for good. The new presidential administration’s relentless attack on federal spending related to TB research and science seriously threatens this progress, betraying people affected by TB across the world, and in the heartland alike.
Erin McConnell, born and raised in Kansas City, is a senior TB Project associate at Treatment Action Group (TAG) focused on community engagement in research. Kendall Martinez-Wright, raised in Palmyra, Missouri, is the government relations and policy associate at TAG, focusing on federal legislation and budget for HIV, TB, and hepatitis C programs nationally and globally. Elizabeth (Lizzy) Lovinger, born and raised in metropolitan Detroit, is the U.S. and global health policy director at TAG, where she advocates for the policies necessary to end the HIV, TB, and hepatitis C pandemics.