- Women with high brain amyloid-beta showed faster tau accumulation than men in three critical brain regions.
- Among APOE4 carriers, women had significantly faster tau deposits in the inferior-temporal region.
- Sex differences in tau may help explain why women face higher Alzheimer’s dementia risk than men.
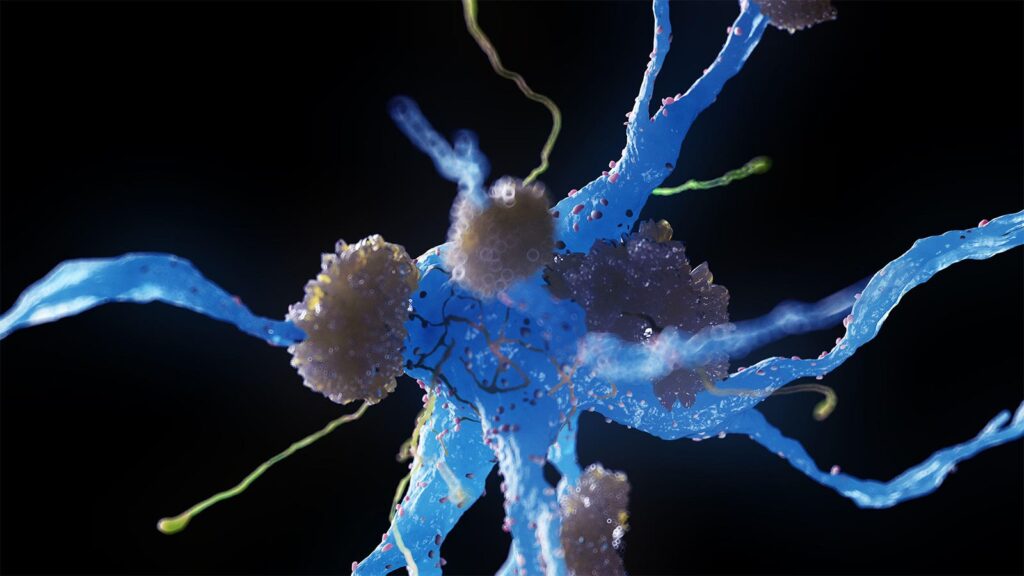
At high levels of brain amyloid-beta, women had more aggressive tau accumulation than men, a meta-analysis of longitudinal PET data showed.
In cognitively normal people with high baseline amyloid, female sex was associated with faster tau buildup over an average of 2.8 years in three brain areas:
- Inferior temporal region (β = -0.14, 95% CI -0.22 to -0.06, P=0.009)
- Temporal fusiform region (β = -0.13, 95% CI -0.23 to -0.04, P=0.02)
- Lateral occipital region (β = -0.15, 95% CI -0.24 to -0.06, P=0.009)
Female sex also was associated with faster inferior-temporal tau accumulation (β = -0.10, 95% CI -0.16 to -0.03, P=0.01) among APOE4 gene carriers, reported Rachel Buckley, PhD, of Massachusetts General Hospital in Boston, and co-authors in JAMA Neurology.
Previous research has shown that tau is higher in cognitively normal women who have similar amyloid levels as men, but most findings have been cross-sectional. While relationships between Alzheimer’s risk and menopause are unclear, studies have demonstrated that a high tau burden occurred in women who had a delay of 5 or more years between menopause onset and the start of hormone therapy.
“When we look at changes over time, we see that women have faster rates of tau accumulation than men in areas of the brain that tend to be most vulnerable to Alzheimer’s disease,” Buckley told MedPage Today. “These changes are much more apparent in women who already have Alzheimer’s risk, such as those who carry the APOE4 gene or those with abnormal levels of amyloid in the brain.”
Once tau starts to accumulate, cognitive decline typically occurs within a couple years, noted co-author Gillian Coughlan, PhD, also of Massachusetts General.
The findings of this study “provide very important insights into the biological mechanisms that may be placing women at a greater risk of Alzheimer’s disease dementia,” Coughlan told MedPage Today. “It’s crucial for us to understand when throughout the lifespan that women start to deposit and accumulate tau. This will help us determine if endocrine factors may be influencing tau deposition and accumulation.”
The meta-analysis used longitudinal data collected between November 2004 and May 2022 from six longitudinal aging and Alzheimer’s studies: the Alzheimer’s Disease Neuroimaging Initiative, Berkeley Aging Cohort Study, BioFINDER 1, Harvard Aging Brain Study, Mayo Clinic Study of Aging, and Wisconsin Registry for Alzheimer Prevention. The analysis assessed seven tau PET outcomes across temporal, parietal, and occipital lobes.
The studies included 1,376 participants without cognitive impairment; about half (55%) were female. The mean age at the first tau scan was 71.9 years.
Overall, 401 participants (29%) had high baseline amyloid-beta and 412 people (30%) were APOE4 carriers. Males and females had similar frequencies of high baseline amyloid, APOE4 status, and mean tau PET follow-up time (an average of 2.8 years).
A major limitation of the study was the lack of racial, ethnic, educational, and other diversity across cohorts, the researchers acknowledged. In addition, it’s possible that a sex-specific tau response to amyloid is propagated by unknown variables like menopause, inflammation, or cardiovascular risk, they pointed out.
The meta-analysis is the largest longitudinal tau PET study ever conducted and highlights that links between sex and tau are present in preclinical Alzheimer’s stages, Buckley and colleagues noted.
The findings also suggest that the disproportionate rates of Alzheimer’s disease among women are driven not only by survival bias but also by an elevated female risk for tauopathy, they added.
“Our next steps are to try to understand when this difference in tau starts to emerge in the disease process. We can see that older women have higher levels of tau than older men and we can now see that they accumulate more rapidly,” Buckley said.
“But what we still don’t know is the point at which they start to diverge — how early in the process does this appear? Answering this question might help us understand what might be knocking women onto a different pathological risk path.”
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
The cohorts in this meta-analysis were supported by the NIH and through contributions from nonprofit groups and industry.
Buckley reported grants from NIH during the conduct of the study. Coughlan reported funding from an NIH award and an Alzheimer’s Association research fellowship.
Co-authors reported relationships with NIH, the Alzheimer’s Association, and private industry.
Primary Source
JAMA Neurology
Source Reference: Coughlan GT, et al “Sex differences in longitudinal tau-PET in preclinical Alzheimer disease: a meta-analysis” JAMA Neurol 2025; DOI: 10.1001/jamaneurol.2025.0013.
Please enable JavaScript to view the