It began with a burning pain in her right eye. At first, Elisabeth Cohen thought she’d gotten something in it. But the next day, as she was pushing her hair back on that side of her head, she noticed a blister near the hairline. She knew immediately what it was: shingles.
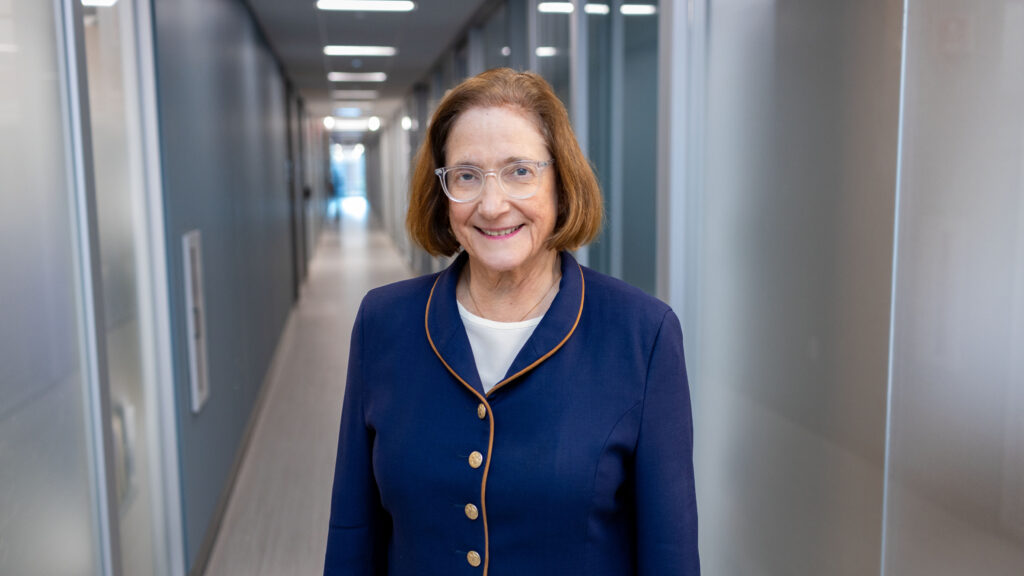
At the time, in 2008, Cohen was director of the Cornea Service at Wills Eye Hospital in Philadelphia. During her three decades there operating on patients’ eyes, she had seen more than enough to know that the clock was now ticking.
advertisement
Shingles is caused by the varicella zoster virus, or VZV — the same herpesvirus that causes chickenpox. After a person has chickenpox, VZV burrows into the nervous system and slips into a smoldering latent state. As they get older and their immune system weakens, VZV can reactivate. If that happens in the nerves that reach across the skull and forehead, the virus can also get into the eye and cause ulcers and scarring on the cornea — the clear covering at the front of the eye that keeps out dust and harmful ultraviolet radiation and also focuses light onto the lens behind it.
Around 8% of people who suffer an episode of shingles will get an infection in the eye, a condition known as herpes zoster ophthalmicus, or HZO. About 1 in 10 HZO cases result in moderate to severe vision loss. In all cases, that damage is permanent.
Cohen was in this unlucky group, despite catching it early and receiving immediate treatment. Thirteen months after that first blister appeared, vision in her right eye had deteriorated to the point that she no longer had the depth perception to perform surgeries. At the NYU Grossman School of Medicine and NYU Langone Health, where she has been since she stopped seeing patients in 2010, Cohen has been working to understand if existing, low-cost antiviral drugs could reduce the risk of vision loss from a shingles infection.
advertisement
At the annual meeting of the American Academy of Ophthalmology over the weekend, she presented promising data from ZEDS, a $15 million trial she’s been coordinating across 95 medical centers in the U.S. Canada, and New Zealand. The new research shows that after a year of low-dose valacyclovir, patients had a 26% reduction in their risk of having new or worsening eye disease.
Cohen spoke with STAT to discuss the results and their implications for treating HZO and other shingles complications. This interview has been edited for length and clarity.
Tell me about your interest in shingles — did it all start with your own experience with the disease?
I’ve always been interested in infectious diseases. I was a regional principal investigator for the Herpetic Eye Disease Study (HEDS) that was done in the ’90s, which showed that a year of low-dose antivirals reduced episodes [of herpes simplex virus infections in the eye]. And so after I stopped being able to see [out of the right eye] in 2010, I had the idea to try treating herpes zoster the same way. That was the idea behind this study, ZEDS, and now, 14 years later, the study is done.
Even by clinical trial standards, that’s quite the wait. Why did it take so long?
It was crazy because it seemed like such a simple idea. We had evidence from years before that active virus replication was involved with the complications of shingles in the eye. If it worked with herpes simplex disease, why not try it with herpes zoster eye disease? But at that point, I thought my career was ending. I was leaving a big practice and moving to New York to be with my husband who lived there. So I gave this idea to a friend of mine at UCSF [University of California, San Francisco] where they had led the HEDS study, and he did one survey that found a lot of interest and that was the end of that.
And then in 2012, right after Hurricane Sandy, things were kind of quiet at NYU, and my husband said, “You have time to do this, just do the grant yourself.” I had 60 participating clinical centers all ready to do the study when I first submitted in September 2013, and that got rejected by the NEI [National Eye Institute], and then the second submission got rejected too. And it was quite frustrating because people didn’t seem to be knowledgeable on the subject.
advertisement
I actually spoke to someone at NEI afterwards and complained, because in the review people were misquoting papers I had written. And he pointed out to me that one-third of the NEI budget went to the disease I was talking about. And I’m like, “I don’t think so, I think you’re thinking of Herpes simplex eye disease.” I explained this was caused by a different herpesvirus, the chickenpox varicella zoster virus. After that they were more receptive. We got funded in 2016 and our first participant was enrolled in the fall of 2017.
I’m struck by the lack of expertise, even somewhere like the NEI, about this virus. What’s going on there?
Well, it is a harder virus to study. There are not animal models for varicella zoster disease. But you know, after we were told that there was so much research being done at NEI, we realized there was somewhere we could go and find out all the supported research being done at NIH, and at that point only a very small amount was being done on zoster at the Institute of Aging. So it’s been kind of ignored compared to herpes simplex.
That’s surprising given that shingles has been on the rise for decades. But I guess, it also doesn’t seem to get the same kind of attention that other diseases of aging do.
Well, there’s a real misconception that it’s a disease of old people. And you know, the definition of old is like, “older than you.” But in general, half of the cases come in people under the age of 60. And that was the first paper I wrote after I got it because I myself thought I was too young to have this problem. And although it’s more common and severe in people who are immunocompromised, still, over 90% of the people getting shingles are basically healthy.
That’s the other frustrating thing to me; we have had a really effective vaccine since 2017 that’s been approved for people aged 50 and above. And yet the most recent data is that only 12% of people in their 50s have gotten vaccinated.
Why do you think that is — is there maybe a sense out there that shingles is more of a rare or not super-serious thing?
advertisement
Well, I don’t know but it is not rare and it is serious. One in three people in the U.S. will get shingles in their lifetime. And if you live to age 85, it goes up to one in two. There are over 1 million new cases of shingles per year in the United States. And shingles can be complicated by strokes, which is potentially more common after the involvement of the eye. That’s because the virus moves directly from nerves to vessels and those vessels become inflamed, and if those vessels are in your brain, that can result in a stroke.
People who get shingles when they’re over the age of 65 are more likely to have the chronic pain syndrome that can be a complication of the disease. But the other complications — like eye disease or if it goes to your ear, hearing disease — those kinds of complications are just as common in younger people.
So I think doctors really need to be more strongly encouraging the use of this vaccine because adults generally do follow the advice of their doctors and the vaccine is available at pharmacies. At least 15% of people get side effects [from the vaccine] like a sore arm and flu-like symptoms, which can interfere with normal activities, and you need two doses, so you’ve got to be prepared after each dose to be sick and sore. But it’s an effective vaccine that right now is very much underutilized.
All right, so let’s talk about that study that you’ve now spent at least 14 years of your life on — what did you learn?
So, the most significant results were that we could reduce the likelihood of new or worsening eye disease significantly, at 18 months. We did not reach significance at 12 months. But for both 12 and 18 months we did significantly reduce multiple flare-ups of the eye disease, which is very important, because it’s these flare-ups that go on to become chronic disease and a loss of vision.
We were also able to reduce the amount of neuropathic pain medications that our patients needed who were on valacyclovir compared to placebo. And these neuropathic pain meds are not well-tolerated. I know this from having tried them myself for the acute pain I had. They make people very drowsy. I was put on a super low dose at bedtime and had trouble thinking straight. And I had patients who were prescribed megadoses and in retrospect, I think they were being given so much medicine so that they wouldn’t be able to complain any more about their pain because they were so tired.
advertisement
So how do you think these findings should change how doctors treat patients going forward?
My hope is that a lot of ophthalmologists are going to give their zoster patients the recommended high dose of the oral antiviral, for 7 to 10 days, and then follow that by one year of a low dose, to try to reduce the likelihood of more episodes of eye disease as well as to decrease the need for pain medicine.
Should this spur taking a closer look at how these low-dose antivirals might be used for other complications of this disease?
That’s going on already. The most recent area of interest that’s striking to me is about dementia prevention.
We’ve written about some of these new studies showing that not only is shingles associated with dementia, but also that getting a shingles vaccine can significantly lower the risk of developing dementia later.
The remarkable thing about the study in Wales was that they were using the original Zostavax vaccine, which loses efficacy after several years. And they gave it to people around age 80, when the vaccine was less effective. So it was quite remarkable that they showed benefit with regard to the subsequent development of dementia. So I think it’s going to be further studied. It’s quite intriguing.