- Disrupted circadian rhythms in cognitively normal adults were tied to higher subsequent amyloid-beta levels.
- The relationship was stronger in APOE4 carriers.
- The findings remained largely similar after excluding participants with baseline Alzheimer’s pathology.
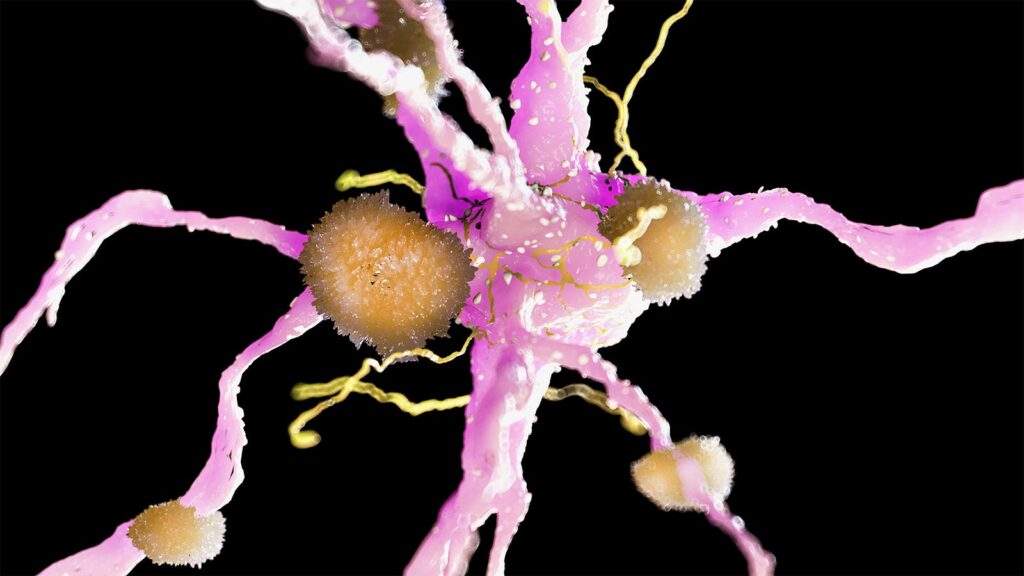
Disrupted circadian rhythms in cognitively normal adults were tied to higher subsequent amyloid-beta levels, prospective data showed.
Higher daily variability at baseline — an indicator of fragmented 24-hour activity rhythms — was associated with higher PET amyloid burden 8 years later (β=0.15, P=0.02) after adjusting for age, sex, APOE4 status, and other factors, according to Julia Neitzel, PhD, of Erasmus University Medical Center in Rotterdam, the Netherlands, and co-authors.
The relationship was stronger in APOE4 carriers (β=0.38, P=0.03), Neitzel and colleagues reported in JAMA Neurology. The findings remained largely similar after excluding participants with baseline Alzheimer’s pathology.
Earlier research has suggested the relationship between Alzheimer’s and sleep may be bidirectional and could span several decades.
“The literature on sleep and Alzheimer’s disease pathology is very inconsistent,” Neitzel noted. “However, the main difference between this study and other research was that we controlled for Alzheimer’s disease pathology at baseline,” she told MedPage Today.
“When we excluded participants with a positive Alzheimer’s blood test at baseline, we still found an association between higher 24-hour rest-activity rhythm fragmentation at baseline and Alzheimer’s PET burden at follow-up,” Neitzel added. “This suggests that fragmentation is likely to be a risk factor, rather than a result, of Alzheimer’s disease pathology.”
According to the Lancet Commission, about 40% of dementia cases may be prevented or delayed by modifying 12 key risk factors. At this point, sleep is not one of them.
“Considerable interest surrounds the role of sleep dysfunction in the development of Alzheimer’s disease and dementia,” observed Matthew Pase, PhD, of Monash University in Victoria, Australia, who wasn’t involved with the study.
“If poor sleep contributes to dementia, improving sleep symptomatology could be one strategy to lower dementia risk,” he told MedPage Today.
Previously, the Rotterdam study did not find an association between fragmented 24-hour activity rhythms and incident dementia, Pase noted. But the current study — which looked at Alzheimer’s biomarker changes that occur years before dementia onset — adds to the growing evidence that circadian disruption may increase dementia risk, he said.
In this analysis, Neitzel and co-authors evaluated sleep and 24-hour activity rhythms from 319 participants in the prospective Rotterdam study. No one had a diagnosis of dementia at baseline. At a mean follow-up of 7.8 years (from 2018 to 2021), the researchers measured amyloid burden on PET.
Mean baseline age was 61.5 years; mean age at follow-up was 69.2. About half (47%) of participants were women.
Sleep and activity were assessed by actigraphy for 7 days and nights to determine objective sleep and 24-hour activity rhythms. Participants also maintained diaries to self-report their sleep patterns. Plasma assays assessed baseline amyloid-beta 42/40 ratios and phosphorylated tau (p-tau)181 and p-tau217 levels.
While higher fragmentation of 24-hour activity rhythms was associated with more severe amyloid pathology at follow-up, no other objective or self-reported measure of sleep was, Neitzel and colleagues reported. There was no strong relationship between sleep duration and amyloid pathology, contrary to what some earlier research has shown.
“Self-reports of shorter sleep duration were associated with increased amyloid-beta pathology in most but not all studies,” they wrote. “However, this association has not been confirmed in previous actigraphy studies, consistent with the current findings.” Different sample sizes may be one underlying reason; actigraphy studies are typically smaller because they are more burdensome than self-reports, they added.
Because participants had only one PET scan, longitudinal analyses were limited in the study. The gold standard for measuring sleep is polysomnography, though actigraphy “shows fair associations with polysomnography,” the researchers noted. And while possible sleep apnea was assessed through self-reports, it still may have influenced results.
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
This project received funding from the European Union’s Horizon 2020 program, ZonMW, the Alzheimer’s Association, the public-private partnership ABOARD, Topsector Life Sciences & Health, and the Tailored Activity Program (TAP)-dementia.
Neitzel and co-authors reported no conflicts of interest.
Pase reported relationships with the National Institute on Aging, the National Health and Medical Research Council of Australia, and the Alzheimer’s Association.
Primary Source
JAMA Neurology
Source Reference: Ho PTN, et al “Sleep, 24-hour activity rhythms, and subsequent amyloid-β pathology” JAMA Neurol 2024; DOI: 10.1001/jamaneurol.2024.1755.
Please enable JavaScript to view the