As pediatricians who take care of children in the inpatient, emergency, and primary care settings, we are alarmed by the recent trend of families having to go without basic medications to control their child’s asthma. At least seven children have died due to uncontrolled asthma this year in the Philadelphia region, a dramatic increase from prior years. At our institution, admissions for intensive care to support children with asthma have nearly doubled from the pre-pandemic baseline, and admissions for asthma are up 50% in March and April compared to last year.
This increase in child asthma acuity and deaths is likely multifactorial, but access to basic medications is one modifiable driver. Limited access stems from three main issues: the discontinuation of a common branded asthma medication, lack of insurance coverage for its generic alternative, and shortages of a similar branded alternative.
advertisement
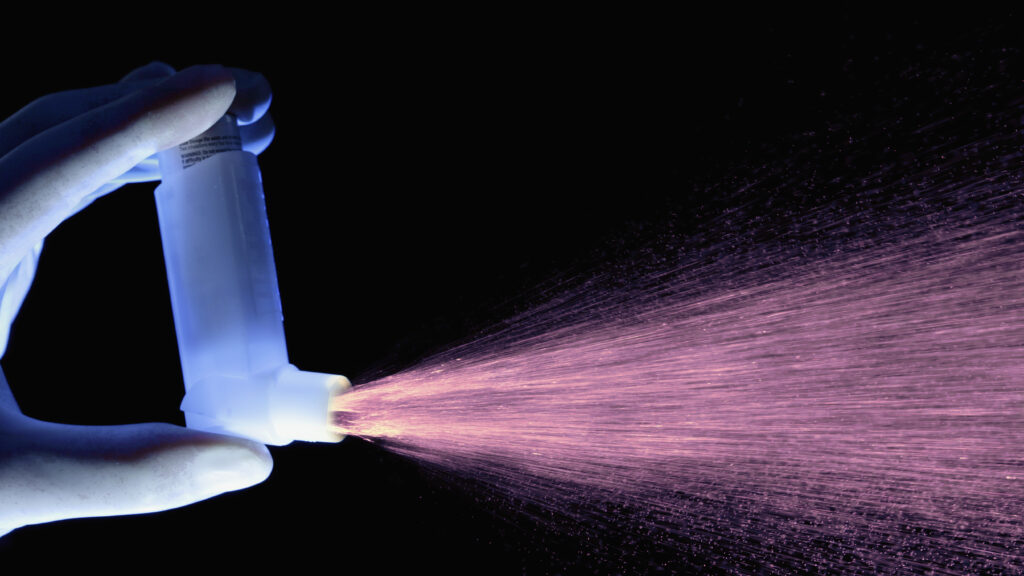
In January 2024, GSK discontinued making Flovent, one of the most commonly prescribed inhaled asthma maintenance medications in the U.S. Although the company continues to make a generic medication with the same active compound, fluticasone propionate, this seemingly simple transition has led to a tremendous disruption in the care of children with asthma because of the second problem: lack of insurance coverage of this generic alternative.
We are now regularly seeing children who require repeat hospitalizations and ED visits because their needed controller medicine is not covered by insurance and therefore the asthma gets out of control. A mother told one of us (B.B.), “I don’t understand. My son needs this medication. How can the insurance company not cover it? What are we supposed to do?” The family had been without an asthma controller medication, as the prescribed generic alternative to Flovent was not covered by his insurance.
Normally, in the event of a change like Flovent’s discontinuation, doctors can simply switch a prescription to the generic alternative without interrupting the daily medication regimen families are accustomed to. In fact, health systems and doctors include the default language — “or generic equivalent” — on electronic prescription templates, allowing pharmacies to automatically switch patients to a generic equivalent. In the best-case scenario, the switch from Flovent to generic fluticasone could have been made automatically.
advertisement
But in the transition away from Flovent, some large insurers and their pharmacy benefit managers (PBM) — both commercial and Medicaid — made a decision not to cover generic fluticasone. This decision was made on cost, as several FDA-approved alternatives in this class of medicines, called inhaled corticosteroids, are cheaper than generic fluticasone. This is a practice called non-medical formulary switching, which typically occurs when a PBM changes coverage to an alternative drug for which it can negotiate a better price, but is not necessarily better for patients.
Non-medical formulary switching is frustrating to families and providers, and has been shown to be associated with harmful effects, particularly for people whose conditions are well controlled. It is particularly challenging for children with asthma who are under 8 years old, as they are not able to take many of the breath-actuated or dry powder inhalers designed for adults, leaving them with limited alternatives.
This brings us to a third problem: substantial shortages of Asmanex, a branded asthma controller that’s similar to Flovent. Nearly five months after Flovent’s discontinuation, it remains nearly impossible nationally to find Asmanex.
Yet even in the face of this shortage, many PBMs have persisted in their requirements for prior authorization, which often requires several days for a medication to be approved following repeated attempts by doctors to get it approved.
When patients and their families need an asthma controller medication, doctors now face the difficult choice of waiting several days for the insurance company to approve a medication that actually does work and is familiar to families or prescribing a medication that may be difficult for a child to take. If the prescription is denied, prescribers must identify an alternative inhaler that is covered but may be less effective, then try to teach the child and family how to use a different kind of inhaler.
There is something insurance companies and state Medicaid offices can do right now to ease the burden on families and children: cease prior authorization requirements on all inhaled steroids (such as generic fluticasone) used for asthma treatment until the medication shortage has abated.
We worked with the team that manages the Pennsylvania Medicaid common formulary to make this adjustment for the youngest children, and appreciate their responsiveness to this issue. This is an important first step that other commercial insurers and state Medicaid offices should immediately institute with their PBMs. What’s needed longer term is a pharmacy benefit process that allows patients streamlined access to the medications that work for them without unnecessary barriers on prescribing or fulfillment.
Reducing barriers to these critical medications can prevent more unnecessary hospitalizations, intensive care treatment, and deaths related to untreated asthma. It’s unconscionable that children should die of uncontrolled asthma in the U.S. when there are cheap and effective medications available to control this disease.
Chén Kenyon is a pediatric hospital medicine physician and population health researcher. Bianca Nfonoyim Bernhard is an emergency department pediatrician. Tyra Bryant-Stephens is a primary care pediatrician and asthma researcher.