
The Persistent Challenge of Healthcare Access and Cancer Screening Disparities
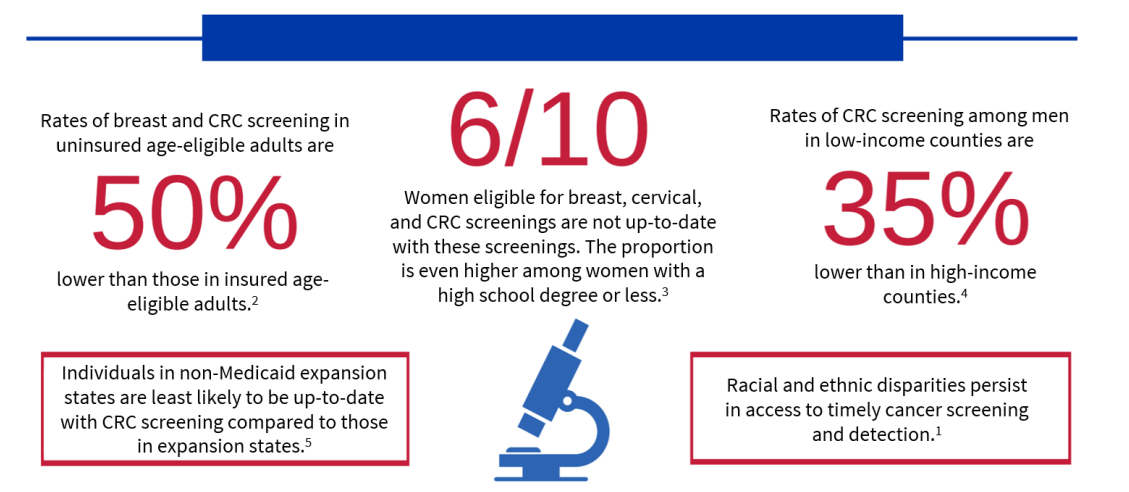
In the United States, the healthcare landscape remains plagued by significant disparities, particularly for underserved populations. People of color, low-income families, rural residents, and immigrant communities often face a daunting array of barriers that prevent them from accessing quality preventive and diagnostic services.
These barriers include limited access to healthcare facilities, financial constraints, transportation difficulties, language and cultural differences, and a lack of awareness about the importance of preventive health measures. The consequences of these disparities are staggering, especially when it comes to diseases like lung cancer.
Early detection through regular screenings is crucial for improving survival rates, but these life-saving measures are often out of reach for marginalized communities. Studies reveal a concerning trend: only a small percentage of high-risk individuals in these communities receive the recommended lung cancer screenings. This translates to delayed diagnoses, advanced stages of disease at the time of discovery, and ultimately, poorer health outcomes.
Specific Case: The Devastating Impact of Lung Cancer and the Urgency for Early Detection
Lung cancer is a particularly insidious disease because it often progresses with minimal symptoms in the early stages. When noticeable symptoms appear, the cancer might have already advanced to a stage where successful treatment becomes significantly more challenging. Early detection through regular screenings is critical to improving survival rates, but access to these screenings remains a significant barrier for underserved communities.
According to the American Lung Association, lung cancer is the leading cause of cancer-related deaths in the United States, claiming over 130,000 lives annually. The five-year survival rate for lung cancer is just 21%, but this number rises to 60% when the disease is detected at an early, localized stage. Unfortunately, only 16% of lung cancers are diagnosed at this stage, largely due to the lack of access to regular screenings in underserved communities.
Did you know that only 5.8 percent of Americans receive their annual lung cancer screenings? Unfortunately, at Federally Qualified Health Centers (FQHCs), other types of cancer are not screened as frequently as you on the chart below.
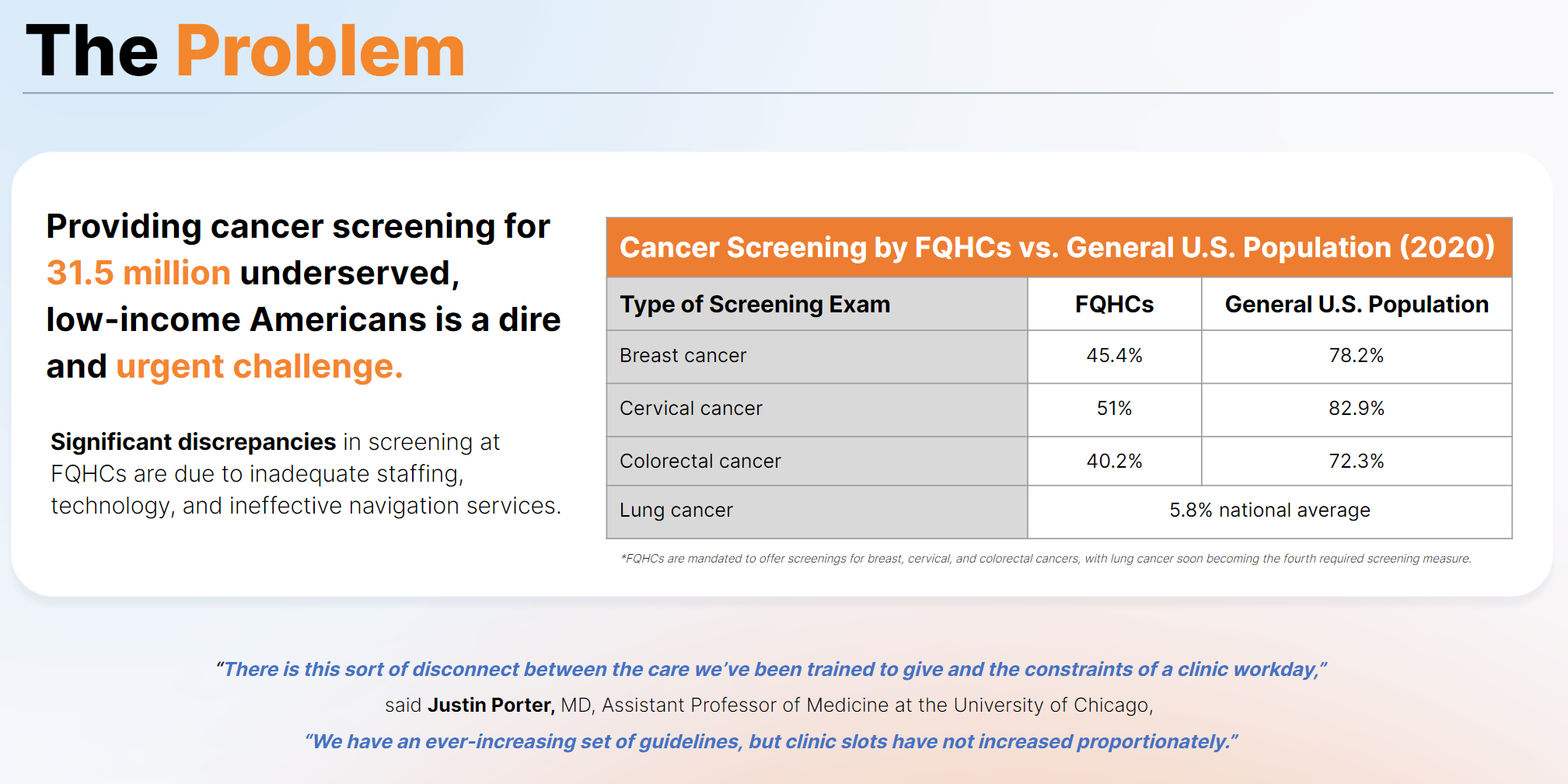
Closing the Gap: The Pivotal Role of FQHCs in Improving Cancer Screening
Federally Qualified Health Centers (FQHCs) are uniquely positioned to play a vital role in bridging the gap in cancer screening for underserved populations. These community-based healthcare providers are designed to offer accessible and affordable primary care services to those who might otherwise struggle to access the healthcare system.
FQHCs can be instrumental in implementing innovative strategies and leveraging available resources to enhance cancer screening rates within their communities. Here are some key areas where FQHCs can focus their efforts:
- Raising Awareness and Education:
- Develop and disseminate educational materials in multiple languages about the importance of cancer screenings, particularly for high-risk individuals, to cater to diverse populations.
- Collaborate with trusted community leaders and healthcare professionals to act as advocates and champions for cancer screening initiatives.
- Organize outreach programs and community events to provide information and encourage participation in screening efforts.
- Streamlining Screening Processes:
- Offer flexible appointment scheduling options, including evenings and weekends, to accommodate the needs of patients.
- Provide transportation assistance, such as shuttle services or gas vouchers, to help patients overcome logistical barriers.
- Ensure clear communication about the screening process, from scheduling to follow-up care, to alleviate concerns or confusion.
- Leveraging Technology for Efficiency:
- Utilize AI-powered platforms, like those offered by Oatmeal Health, to identify high-risk patients within the FQHC’s patient population and optimize screening resources.
- Integrate electronic health records and data analytics to track screening adherence and identify gaps in care proactively.
- Explore using mobile screening units like CT scan vans or mammo buses to bring critical services directly to underserved communities.
- Building Partnerships:
- Collaborate with local hospitals, imaging centers, and patient advocacy groups to expand the services available to FQHC patients.
- Establish partnerships with mobile screening units and telemedicine providers to enhance cancer screening and follow-up care access.
- Engage with pharmaceutical and biotech companies to explore innovative solutions, such as liquid biopsy tests or at-home phlebotomy services that can further reduce barriers to screening.
- Addressing Social Determinants of Health:
- Assist with childcare or work leave to facilitate attendance at screening appointments.
- Address financial concerns related to co-pays or transportation costs to ensure cost is not a barrier to accessing screenings.
- Ensure culturally competent communication and navigation support to overcome language and cultural barriers.
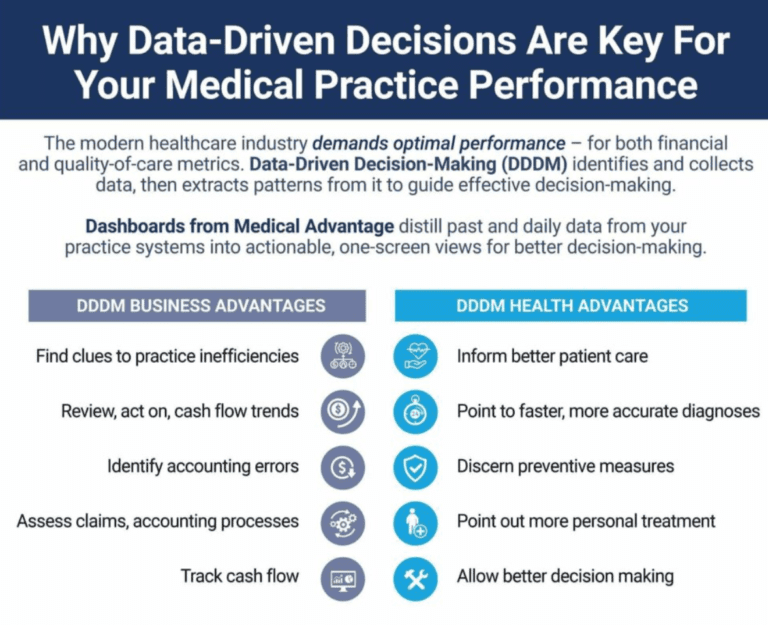
Monitoring Progress and Making Data-Driven Decisions: The Power of UDS Metrics
The National Health Service Corps (NHSC) utilizes Uniform Data System (UDS) metrics to track the performance of FQHCs. These metrics serve as valuable tools for FQHCs to assess the effectiveness of their cancer screening initiatives and make data-driven decisions to drive continuous improvement.
Key UDS metrics relevant to cancer screening include:
- Preventive Care and Screenings (PCS):
- This metric tracks the number of preventive services delivered, including cancer screenings.
- By monitoring PCS data, FQHCs can identify areas for improvement and tailor their strategies to increase cancer screening rates.
- Cancer Diagnoses:
- Analyzing trends in cancer diagnoses among FQHC patients can help assess the effectiveness of prevention and early detection efforts.
- Quality of Care:
- UDS metrics related to quality of care can reveal areas where FQHCs can enhance patient education, communication, and overall management of cancer screening programs.
Leveraging these UDS metrics, FQHCs can make informed decisions, allocate resources more effectively, and continuously refine their strategies to improve cancer screening rates and health outcomes within their communities.

The Power of Innovation: Expanding Access through AI-Enabled Mobile Screening Units, Cancer Screening/Liquid Biopsies, and At-Home Phlebotomy
As the healthcare landscape evolves, new technologies and innovative approaches hold immense potential for enhancing accessibility to cancer screening services, particularly for underserved populations.
- Mobile CT Scanners and Mammo Buses:
- These mobile screening units can bring critical services, such as low-dose CT scans for lung cancer and mammograms for breast cancer, directly to underserved communities, eliminating transportation barriers.
- By partnering with FQHCs and local healthcare providers, these mobile units can reach individuals who might otherwise forgo or delay their cancer screenings.
- Liquid Biopsy Tests:
- Emerging liquid biopsy technologies have the potential to detect cancer through a simple blood draw, reducing the need for more invasive procedures.
- As these tests continue to be developed and validated, FQHCs can explore incorporating them into their cancer screening programs, further increasing accessibility and reducing patient barriers.
- At-Home Phlebotomy Services:
- For patients who cannot visit an FQHC, home-based blood draws for liquid biopsies or other diagnostic tests can be facilitated by partnering with qualified phlebotomy providers.
- This approach can help reach individuals with mobility challenges, transportation difficulties, or other barriers to accessing traditional healthcare settings.
- Artificial Intelligence:
- Machine Learning (ML): ML algorithms can predict disease outcomes by analyzing patient data, enabling personalized treatment plans.
- Computer Vision: Computer vision aids in medical imaging analysis, improving the accuracy and speed of diagnosing conditions such as tumors.
- Generative Adversarial Networks (GANs): GANs can generate high-quality synthetic medical images to train radiologists and enhance diagnostic tools.
- Generative AI: Generative AI creates synthetic data for training other AI models, enhancing the robustness and reliability of healthcare AI applications.
- Large Language Models (LLMs): LLMs assist in medical research by rapidly analyzing vast amounts of medical literature to provide insights and recommendations.
By embracing these innovative solutions, FQHCs can significantly expand their reach and ensure that underserved communities have access to life-saving cancer screening services, ultimately improving early detection and health outcomes.

Conclusion: Bridging the Gap Through Collaborative Efforts
Addressing the persistent challenge of healthcare disparities and improving cancer screening rates in underserved communities requires a multifaceted approach. FQHCs, with their deep roots in the communities they serve, are uniquely positioned to lead the charge in bridging this gap.
By implementing targeted strategies, leveraging technological advancements, and forging strategic partnerships, FQHCs can make significant strides in enhancing access to cancer screening services and, ultimately, saving lives. The key lies in a comprehensive approach that encompasses raising awareness, streamlining processes, utilizing data-driven insights, and addressing the social determinants of health.
Through this collaborative effort, FQHCs can empower underserved populations, provide hope, and ensure that everyone, regardless of their background or socioeconomic status, has access to the quality healthcare they deserve. Together, we can turn the tide on health disparities and create a more equitable future where all early detection and life-saving interventions are within reach.
About Jonathan Govette
Jonathan Govette, Founder and CEO of Oatmeal Health, uses his expertise in healthcare technology to advance AI-driven cancer screening and biotech solutions for underserved populations. With a background in pioneering SaaS referral platforms and over 200 healthcare publications, he partners with leading healthcare institutions to promote health equity. Through Oatmeal Health’s integrated primary care and radiology platform, he ensures early diagnosis and delivers clinical care and cutting-edge technology to Federally Qualified Health Centers (FQHCs).

