What You Should Know:
– Candid Health, the innovative revenue cycle automation platform designed for healthcare providers raises $29M in a Series B funding round led by 8VC, with participation from existing investors First Round Capital, BoxGroup, and Y Combinator.
– This latest investment brings the company’s total funding to $47M.
Simplifying Medical Billing, Empowering Providers
Candid Health is committed to simplifying the complex and often frustrating process of medical billing, enabling healthcare providers to focus their time and energy on delivering exceptional patient care. The current U.S. healthcare system, with its myriad of payors and ever-changing requirements, results in a staggering $280B in annual costs. Manual billing processes are slow, error-prone, and ripe for automation.
Transforming Billing with Automation
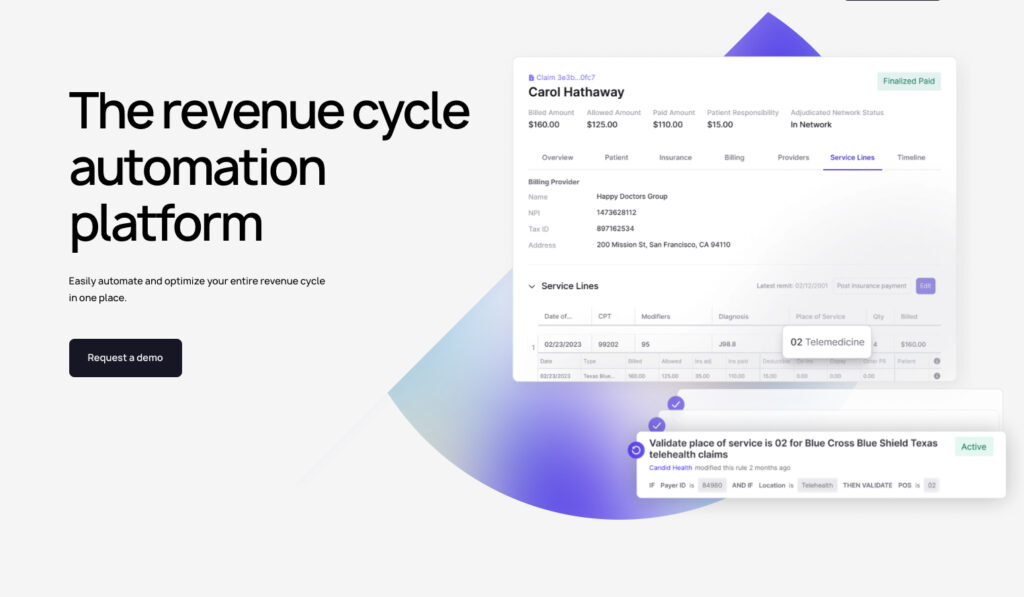
Traditional technologies have struggled to adapt to the dynamic regulatory landscape and the intricacies of the claims cycle. Candid Health’s advanced platform leverages automation to revolutionize the entire billing process, from initial claim submissions to accounts receivable management. This eliminates manual interventions and empowers the system to auto-correct claims, ensuring accuracy and efficiency.
Tangible Results for Customers
The impact of Candid Health’s platform is evident in the success of its more than 150 customers. High-performing clients consistently achieve remarkable first-pass resolution and net collection rates of 95-99%, guaranteeing accurate payment the first time around.
“Most medical billing companies focus on resolving issues post-claims submission more efficiently, but we’re flipping the model. We focus on submitting claims correctly the first time so that there are no issues to fix,” said Nick Perry, CEO and co-founder of Candid Health. “We’ve been rethinking medical billing from the ground up to automate complexity. This ensures healthcare providers can get paid, on time, and for less cost.”