What You Should Know:
– CentralReach, a provider of Autism and IDD care software, is transforming revenue cycle management (RCM) with the launch of two innovative AI-powered solutions: CR ClaimCheckAI™ and the upcoming CR ClaimAgentAI™.
– The AI tools address critical challenges faced by ABA and multidisciplinary organizations, such as increasing profitability and optimizing cash flow, despite staffing shortages and financial constraints.
CR ClaimCheckAI: Intelligent Claims Auditing
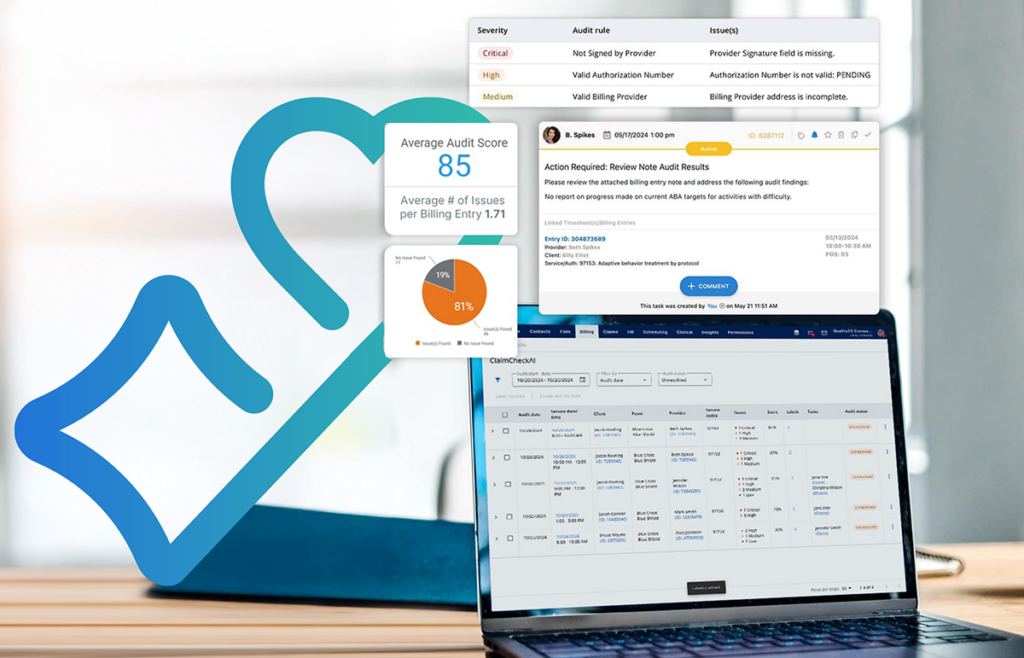
CR ClaimCheckAI leverages artificial intelligence and a comprehensive library of payor-specific rules to audit claims with unparalleled accuracy. This solution offers:
- Proactive Issue Detection: Identifies potential claim issues before submission, reducing denials and rework.
- Interactive Dashboard: Provides real-time insights into claims data, processing, and trends, enabling data-driven decision-making.
- Seamless Workflow Integration: Embeds claim issue resolution directly into CentralReach’s task manager, streamlining workflows and improving efficiency.
- Performance Benchmarking: Delivers a Clean Claims Score, allowing providers to compare their performance against industry standards.
CR ClaimAgentAI: Automated Claims Processing
Coming in Q1 2025, CR ClaimAgentAI will further revolutionize RCM by automating the entire claims process. Powered by CentralReach’s proprietary AI agent, cari™, this solution will:
- Generate, audit, and submit claims automatically, freeing up staff for more critical tasks.
- Increase clean claim rates and accelerate reimbursement.
- Improve operational efficiency and reduce administrative burden.
- Enhance transparency by providing a clear view of the claims process.
“With increasing compliance mandates and payor scrutiny, improving claims performance is top of mind for all providers in the Autism and IDD Care market. Current solutions like ad hoc manual checks, outsourcing to offshore RCM service providers, or the use of clunky, disconnected third-party point solutions, do not enable providers to improve performance without significant learning curve requirements and manual processing that blunt the purported ROI of those solutions. CR ClaimCheckAI and our soon to be released ClaimAgentAI offers all the benefits of the most sophisticated LLM-based solutions with the convenience of having that solution built into the UI and daily workflows that their teams already use and love,” said Chris Sullens, CEO of CentralReach. “CR ClaimCheckAI when paired with CR ClaimAgentAI will offer the benefits of third-party RCM service offerings at a fraction of the cost, creating significant ROI for our customers in a critical area of their business – greatly enhancing clean claims rates from the outset, accelerating reimbursements, and reducing operational burdens, allowing providers to scale their services faster and more effectively.”