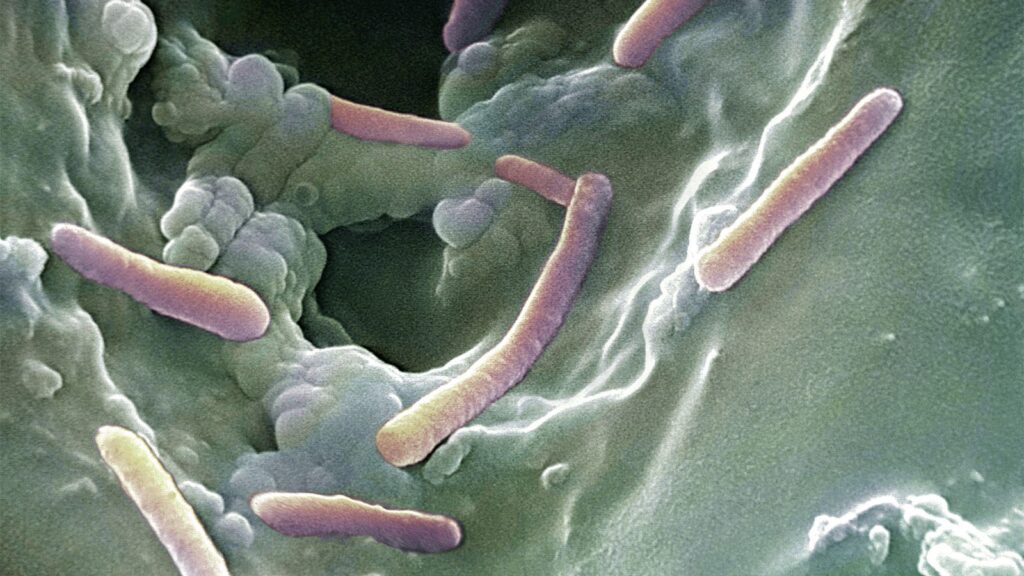
- Lung transplant recipients are highly susceptible to infection, and Pseudomonas aeruginosa is a leading cause of bacterial pneumonia for them.
- After lung transplantation, infection with P. aeruginosa independently predicted antibody-mediated rejection.
- Early detection of infections was suggested as a way to predict the development of antibody-mediated rejection and to develop treatments to prevent or treat antibody-mediated rejection.
After lung transplantation, infection with Pseudomonas aeruginosa independently predicted antibody-mediated rejection (AMR), researchers found.
Individuals found to carry the bacteria after receiving a new lung had a more than four-fold increased risk of developing definite AMR (HR 4.09, 95% CI 1.75-9.54, P=0.001) and nearly three-fold elevated risk of probable AMR (HR 2.78, 95% CI 1.47-5.27, P=0.002), Andrew E. Gelman, PhD, of Washington University School of Medicine in St. Louis, and colleagues reported in Science Translational Medicine.
After adjusting for diagnosis of cystic fibrosis and multiple other factors, the risk remained doubled with isolation of P. aeruginosa in respiratory specimens (HR 2.01, 95% CI 1.05-3.85, P=0.035). Isolation of other common respiratory bacteria, including Aspergillus, Gram-positive cocci, and non-Pseudomonas Gram-negative bacilli, or community-acquired respiratory virus was not associated with increased AMR risk.
Through a series of mouse-model studies, the researchers showed a mechanism whereby “P. aeruginosa rapidly invaded bronchial-associated lymphoid tissues, which resulted in acute lymphocytotoxicity, including the death of … Foxp3+ CD4+ T cells that are required to suppress AMR.” This led to the spread of B cells that expressed the CXCR3 protein and were highly sensitive to antigens in the donor organs, leading to antibody-mediated rejection of the transplanted lungs. Blocking CXCR3 prevented rejection of lung transplants in mice infected with P. aeruginosa, suggesting a possible therapeutic strategy.
“Early detection of infections … might help to predict the development of antibody-mediated rejection, and subsequent detection of donor-specific antibodies might then indicate the requirement for antibody removal treatment,” Idaira Guerrero-Fonseca, MSc, and Bryan Yipp, MD, MSc, both of the University of Calgary, wrote in an accompanying commentary paper.
AMR is an increasingly recognized form of lung transplant rejection, with a reported incidence of 27%. Even with aggressive treatment, outcomes are “dismal,” Gelman’s group noted, as some 20% of patients die within 30 days, and 80% die within 2 years.
“Identifying better treatments for AMR is a critical unmet need for recipients of lung transplants,” they wrote, but it has been hampered by not understanding the mechanism that triggers this kind of rejection episode.
Lung transplant recipients are highly susceptible to infection, the researchers noted, and P. aeruginosa is a leading cause of bacterial pneumonia for them. Indeed, it was the most frequently isolated bacterial organism from bronchoscopy specimens after transplantation in Gelman’s study, with 33% of patients having at least one positive culture.
To understand whether P. aeruginosa increases the risk of AMR, the researchers retrospectively studied 572 patients who underwent lung transplantation at a single center from January 2008 through December 2016. During study follow up through 2019 for an average 4.92 years per patient, 66 patients developed clinical AMR, which was definite in 35%.
AMR was associated with 5.73-fold elevated risk of mortality (P<0.001), as well as significantly increased risk of chronic allograft dysfunction (HR 3.69) and worse chronic allograft dysfunction-free allograft survival (HR 4.53). Among the 188 who had at least one positive culture for P. aeruginosa, 85 (45%) had cystic fibrosis as the underlying diagnosis, followed by interstitial lung disease (ILD, 24%), chronic obstructive pulmonary disease (COPD, 17%), pulmonary hypertension (2%), other diagnoses (6%), while 5% were retransplant recipients.
Of the 100 total cystic fibrosis patients in the study, P. aeruginosa in respiratory specimens after transplantation was associated with five-fold increased risk of AMR (P=0.034). Results were in the same direction but with lower magnitude not reaching statistical significance among COPD and ILD patients (HR 2.81 and 1.26). Patients with cystic fibrosis had a significantly higher number of positive cultures for P. aeruginosa after transplantation than the other diagnostic groups, which the researchers said suggested more exposure to P. aeruginosa after transplantation.
The lack of significant association between P. aeruginosa-positive culture and AMR among recipients with indications other than cystic fibrosis was deemed likely because of the higher infection rate in patients with cystic fibrosis.
The findings have implications for developing future therapeutic strategies, Gelman’s group suggested.
For example, multiple therapeutic monoclonal antibodies have been developed against the T3SS protein implicated in the team’s mouse-model experiments that promote the translocation of exotoxins into the cytoplasm, and phase II studies are underway in treating inflammatory diseases like rheumatoid arthritis with agents that target inhibition of CXCR3 signaling. “Given the accumulation of CXCR3+ B cells in biopsies from lung allografts with AMR, the development of anti-CXCR3 therapies could be an exciting avenue for the prevention or treatment of this life-threatening complication,” Gelman and colleagues wrote.
One limitation of the clinical study they did was the limited number of biopsy samples from lung recipients with a P. aeruginosa infection history and an AMR diagnosis, which made it challenging to correlate the mechanistic findings with the clinical findings.
Exploration of the roles of antigen-presenting cells and inflammatory cells in the initiation and development of donor-specific antibodies and graft injury during P. aeruginosa infection will require future investigation, Guerrero-Fonseca and Yipp agreed.
It’s an open question whether “treating Pseudomonas infection before or after lung transplant might alter the development of donor-specific antibodies or the progression of antibody-mediated rejection,” they wrote.
“Given the rapid advances in genetically manipulated cellular treatments, such as chimeric antigen receptor-activated regulatory T cells, it is possible that therapeutic regulatory T cells could be given to patients after lung transplantation to restore control over B cells,” they added. “Inhibitors of T-bet could also be developed to target pathologic B cell development after lung transplantation.”
Disclosures
This work was supported by National Institutes of Health grants and by the Cystic Fibrosis Foundation, the Barnes Jewish Foundation, the Maritz Chair for Immunology & Oncology, the Children’s Discovery Institute, The Harold Amos Medical Faculty Development Program, Chuck and Mary Meyers, and Richard and Eibhlin Henggeler.
The researchers disclosed no relevant conflicts of interest.
Guerrero-Fonseca and Yipp provided no information about conflicts of interest.
Primary Source
Science Translational Medicine
Source Reference: Liao F, et al “Pseudomonas aeruginosa infection induces intragraft lymphocytotoxicity that triggers lung transplant antibody-mediated rejection” Sci Transl Med 2025; DOI: 10.1126/scitranslmed.adp1349.
Secondary Source
Science Translational Medicine
Source Reference: Guerrero-Fonseca IM, Yipp BG “No tolerance for Pseudomonas in lung transplants” Sci Transl Med 2025; DOI: 10.1126/scitranslmed.adu6563.
Please enable JavaScript to view the