Though AI has successfully been utilized in healthcare for decades, a Pew Research Center survey revealed that 60% are uncomfortable with their provider relying on AI for their own healthcare.
This dichotomy is therefore likely due in part to a lack of awareness and understanding around the technology. Before the public is forced to understand complex, revolutionary, future-state technological developments in healthcare, they must understand how the technology is safely used today. Examples of this technology in motion include:
- The pulse oximeter, also called a plethysmograph or pleth, uses AI to calculate blood oxygen saturation based on the difference in transmission of red and infrared light in pulsating blood. It was developed in 1972 and widely adopted in clinical practice in the 1980s and 1990s.
- The MRI (magnetic resonance imaging) scanner has been widely used and incorporated AI since the 1980s to detect conditions including brain tumors, multiple sclerosis, strokes, and infections. Modern AI applications for MRI can improve the speed and quality of scans and help with interpretation and diagnosis.
- The echocardiography machine, widely used with AI since the 1980s, uses sound waves to show how blood flows through the heart to search for heart conditions. According to this article in the Journal of Imaging, “Artificial intelligence can use raw echocardiography images/videos to automatically provide structural or functional measurements but also to identify disease states. This ability is based on AI’s capacity to automatically analyze features from images that may be too subtle to be detected by the human eye.”
- AI also can accurately identify normal and abnormal chest X-rays, according to this article and this study.
- Other recent studies show that AI has a 100% success rate in spotting melanomas and a 20% better success rate than human radiologists in detecting breast cancer.
These are just a few of the many AI applications present in medical devices today. Each is an assistive technology that provides accurate measurements to health professionals, enabling them to chart the next steps more effectively. None of the technologies mentioned replace human jobs, but instead, enable healthcare professionals to be more accurate and efficient at their jobs, ensuring the best level of patient care possible.
Beyond using AI for measurements and image interpretation, the next frontiers of AI in healthcare include information systems, some patient interaction, and even possibly robotic surgery. Here are some guidelines to help ensure accurate and safe AI deployments in new applications:
Start With The Back Office
In addition to developing patient-care applications, there is much that AI can do to help with time-consuming back-office administrative tasks that also improve patient care. These include:
- Clinical data abstraction: AI can be used as an assistive technology to automate painstaking and time-consuming data entry, with a required human in the loop to verify accuracy. This enables healthcare professionals to spend more time on patient care, and less on repetitive manual data entry. AI can also mine the hyperscale data sets of clinical registries and share anonymized treatment approaches including comorbidities and medical histories. This can help improve outcomes for current patients with similar conditions to those successfully treated in the past.
- Drafts of clinical summaries: Generative AI systems such as GPT can save time by instantly creating drafts of clinical summaries, also called patient-visit or after-visit summaries, based on physicians’ notes. Generative AI correspondence is also a possibility, but like any AI application in healthcare, should never be sent directly to patients without human review, due to the possibility of inaccuracies or hallucinations.
Only Develop AI Applications That Can Access Sufficient Supporting Data
AI requires statistically significant data to operate; small data sets are insufficient for AI algorithms to be accurate. A condition or procedure that involves only 50 patients per year across the United States won’t provide enough data for AI to evaluate, compute a patient pathway or indicate whether, for example, a treatment is a normal or abnormal practice for the population with that condition. AI applications should operate on vast data sets and as wide a sample of the population as possible.
AI Applications for Patient Care Require Many Trials.
AI applications for patient care should not be immediately dismissed as too risky so that progress is not hampered. There are, however, potential quicker wins with back-office applications versus patient care applications (which generally require many trials before being put into practice). All patient-care AI applications should help clinical professionals do their job, as they are not equipped (and never will be) to replace them. Accuracy is paramount, and a human in the loop is essential to operate and interpret AI applications for patient care.
AI Is Not New
Although AI may be perceived as generally new, it was invented in the 1950s and has been included in software for medical devices since the 1970s. Almost all medical devices include AI software, except purely analog devices such as analog stethoscopes and hypodermic needles. If the public were more aware of facts like these, it is likely that some of the concerns regarding AI use in healthcare may subside.
There currently is an explosion of interest and investment in AI, which is now featured in the marketing materials of most healthcare technology vendors. Before this “AI mania,” which was partially fueled by the launch of ChatGPT in November 2022, AI was usually simply called “software.”
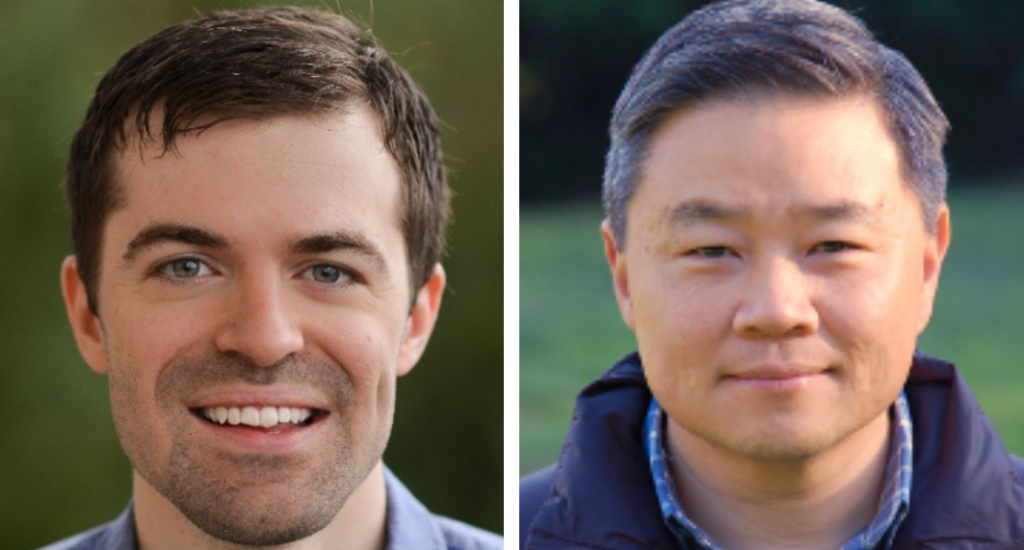
About Matt Hollingsworth
Matt Hollingsworth is the co-founder of Carta Healthcare. His passion for improving patient care developed while helping his mother, a five-time cancer survivor, navigate the U.S. healthcare system and communicate her conditions to providers.
In 2017, Matt Hollingsworth founded Carta Healthcare, dedicated to creating a healthier future by advancing the technology surrounding data practices in healthcare. Today, Carta Healthcare is a leader in delivering improved data-gathering solutions to healthcare systems related to a patient’s diagnosis, treatment, and outcomes. Carta Healthcare’s solutions have revolutionized the processes surrounding registry databases, resulting in markedly faster data collection, superior quality of data, and considerable cost savings for healthcare providers.
Matt holds an MBA from Stanford University, where he also worked in the Systems Utilization Research for Stanford Medicine (SURF Stanford Medicine) lab, researching methods for using information technology to reduce equipment waste and improve patient care. It was through his work at Stanford that he and colleagues founded Carta Healthcare. Before receiving his MBA and founding Carta Healthcare, he was a researcher at CERN (Conseil Européen pour la Recherche Nucléaire) and a member of the team that discovered the Higgs boson, an important discovery in particle physics. Matt received bachelor’s and master’s degrees in physics from the University of Tennessee, Knoxville.
About Dr. Andrew Shin
Andrew Shin, MD, is an Associate Professor in the Division of Cardiology at Lucile Packard Children’s Hospital at Stanford University and the Executive Medical Director, Innovations & Clinical Effectiveness for Stanford Children’s Health. His research has leveraged microsystems, improvement science and high-reliability to better understand the intersection between the quality and efficiency of healthcare delivery. As the Medical Director for Systems Design for Utilization Research for Stanford (SURF MEDICINE), Dr. Shin translates his research to continuously improve the value of healthcare utilizing high-throughput advanced analytics such as machine learning and artificial intelligence. He completed his pediatric residency, along with a dual fellowship in pediatric cardiology and pediatric critical care at Boston Children’s Hospital. Dr. Shin is the Associate Medical Director for Cardiovascular Intensive Care Services and serves as a board member for Pediatric Congenital Heart Association, Carta Healthcare and as liaison for the American Heart Association’s Leadership Committee of the Council on Quality of Care and Outcomes Research.