Two anti-seizure drugs — levetiracetam (Keppra and others) and clobazam (Onfi, Sympazan) — can cause a rare but serious hypersensitivity reaction known as drug reaction with eosinophilia and systemic symptoms (DRESS) that can be life-threatening, the FDA warned Tuesday.
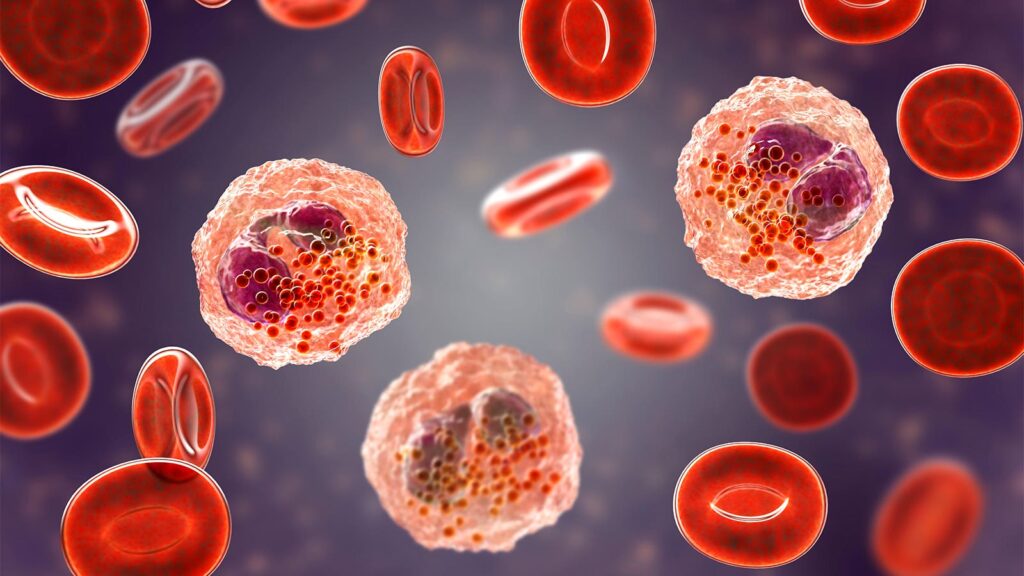
DRESS may start as a rash but can quickly lead to internal organ injury or death, the agency said in a new Drug Safety Communication. The reaction can include fever, rash, swollen lymph nodes, or injury to the liver, kidneys, lungs, heart, or pancreas.
The agency is now requiring warnings about DRESS to be added to the levetiracetam and clobazam prescribing information and patient medication guides.
Levetiracetam was approved in 1999 to control partial seizures, myoclonic seizures, or tonic-clonic seizures in adults and children. Common side effects include unusual irritability or aggression, confusion, loss of balance or coordination, and extreme drowsiness.
Clobazam is a benzodiazepine used as adjunctive treatment for seizures associated with Lennox-Gastaut syndrome in patients at least age 2 years; it was approved in 2011. Common side effects include difficulty speaking or swallowing, tiredness, change in appetite, and problems with muscle control or coordination. DRESS and other serious skin reactions reported generally have been associated only with clobazam and not with other benzodiazepines, the FDA said.
The FDA based its decision on an extensive review that included DRESS cases tied to levetiracetam and clobazam reported to the FDA Adverse Event Reporting System (FAERS) and in medical literature. The search identified 32 serious cases associated with levetiracetam (three in the U.S. and 29 abroad) through March 2023. In all cases, the patients were hospitalized and received medical treatment; in two cases, the patients died. In most cases (25 of 29 cases with treatment discontinuation information), symptoms resolved when patients stopped taking levetiracetam.
The agency also found 10 serious cases linked with clobazam (one in the U.S. and nine abroad) through July 2023. In all 10 cases, the patients were hospitalized and received medical treatment; no deaths were reported. DRESS symptoms resolved in all cases when patients discontinued clobazam.
“Healthcare professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA emphasized. “Diagnosis is often difficult because early signs and symptoms such as fever and swollen lymph nodes may be present without evidence of a rash.”
DRESS can develop 2 to 8 weeks after starting treatment and symptoms and intensity can vary widely, the agency noted. It also can be confused with other reactions like Stevens-Johnson syndrome and toxic epidermal necrolysis.
“Advise patients of the signs and symptoms of DRESS and to stop taking their medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam,” the FDA warned.
Patients should not stop taking levetiracetam or clobazam without first consulting with their healthcare professional, the agency added, as stopping these drugs suddenly can lead to uncontrolled seizures.
More information about DRESS is available from the NIH Genetic and Rare Diseases (GARD) web site and Orphanet.
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Please enable JavaScript to view the