WASHINGTON — As weight loss medications have exploded in popularity, a bill to allow Medicare to cover the drugs has languished virtually unchanged in Congress for a decade.
Until now.
advertisement
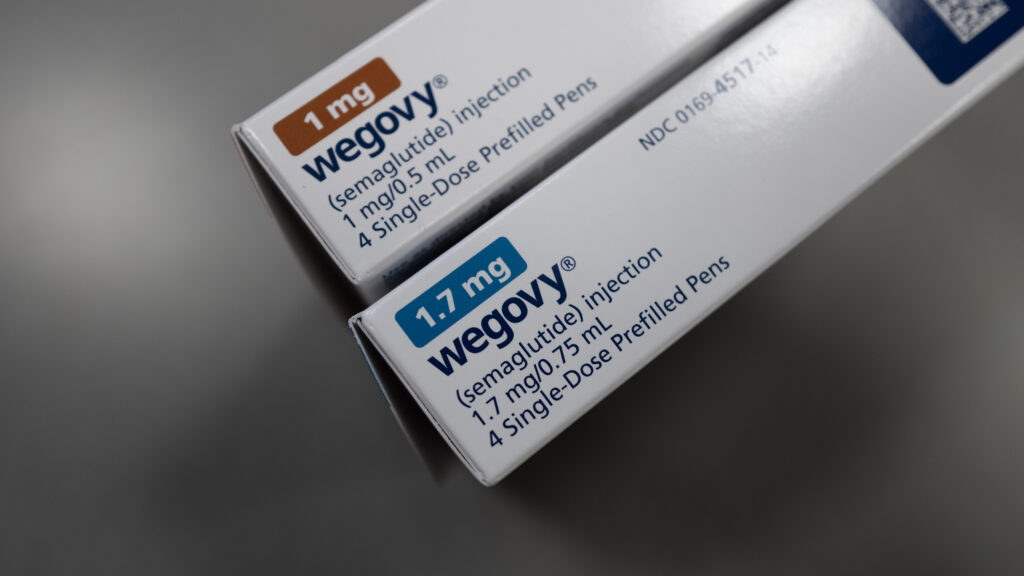
House Ways & Means Committee Chair Jason Smith (R-Mo.) unveiled a proposal on Wednesday to offer a limited pathway for seniors to get their weight loss drugs paid for by Medicare. Right now, Medicare is prohibited from covering medications used for weight loss, like Wegovy and Zepbound.
The new plan is significantly more restrictive than prior proposals. It’s primarily targeted at making sure that people currently taking weight loss drugs don’t get kicked off when they enter the Medicare program, such as by turning 65.
It would only apply to seniors with obesity, while the prior proposal would have extended to seniors who are overweight with a related disease. It would only cover drugs for seniors who had been taking the medications for a year prior to going on Medicare that were paid for by a different insurance plan, and would go into effect in 2027.
advertisement
Those restrictions will, in theory, reduce the cost of the legislation, which has been a roadblock to its advancement for years.
The bill is set for a committee vote Thursday — the first time the bill has reached that milestone. And that means it will likely get cost estimates from congressional scorekeepers that could determine the bill’s fate in an end-of-year spending bill. Proposals that save the federal government money are more likely to hitch a ride than those that cost money.
It’s unclear how much support the scaled-back proposal could receive from House Democrats, or in the Senate.
The new bill also takes a different approach to intensive behavioral therapy to treat obesity. Instead of explicitly allowing therapy to be covered, it instructs Medicare to reconsider its prior coverage decision that limited payment for behavioral therapy to patients with obesity, restricts how many sessions are covered, and requires weight loss progress to continue coverage.