This is Part 2 of “Behind the Counter,” an in-depth video series demystifying the complex world of patents and drug pricing.
The point of prescription drugs is to help people improve their quality of life. When a doctor writes a prescription and sends it along to the pharmacy, oftentimes they’re more focused on the drug’s effectiveness than its cost.
advertisement
But when a patient picks up that drug, the price they will be asked to pay at the counter takes center stage — and it depends on a complex combination of factors. Is it a brand-name or a generic drug? Does the patient have health insurance? If so, does that insurance cover the drug?
Also, how do health insurers decide which drugs to cover, and what amount they’ll cover?
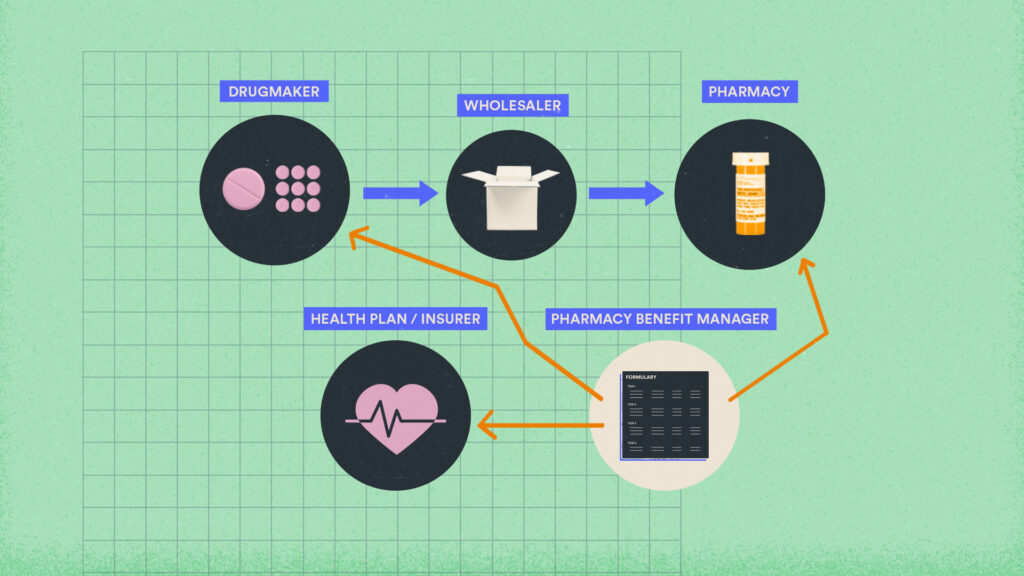
We answer all of these questions in Part 2 of this series. The video outlines what pharmacy benefit managers, or PBMs, are; how formularies and rebates work; and how PBMs use them to mediate with drugmakers, health insurers, and pharmacies in ways that influence the cost of drugs.
STAT’s coverage of patent issues is supported by a grant from the Commonwealth Fund. Our financial supporters are not involved in any decisions about our journalism.
advertisement