Baseline clinical status was markedly different between Black and white patients with Huntington’s disease, data from the Enroll-HD study showed.
Across clinical measures, Black patients with Huntington’s had worse cognitive and motor symptoms at baseline, reported Daniel Claassen, MD, MS, of Vanderbilt University Medical Center in Nashville, Tennessee, and co-authors in Movement Disorders.
Disease progression was similar among race groups.
“Huntington’s disease has long been considered a disease that impacts a predominantly Caucasian population,” Claassen told MedPage Today. “The findings suggest that our outreach efforts to minority patients need to improve.”
The data “indicate that we need to better understand how Huntington’s disease impacts Black patients clinically, as it may have a more severe clinical presentation,” he added.
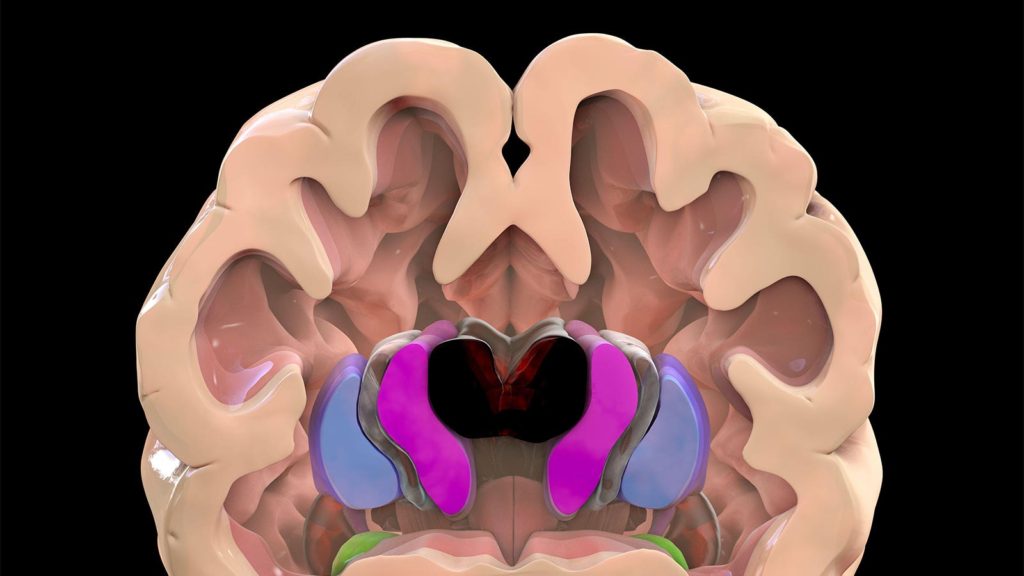
Huntington’s disease is an autosomal dominant genetic disorder caused by extended cytosine-adenine-guanine (CAG) trinucleotide repeats in the huntingtin gene.
Because a child has a 50% likelihood of inheriting the expanded repeat, family-based care may help identify people with Huntington’s, Claassen observed. “We need to change our care model to look after not only the patient, but caregiver, children, and relatives,” he said. “This will allow us to improve our outreach and reduce care disparities.”
Previous research suggested that mistrust in the healthcare system, limited genetic testing, and cultural stigma may have led to less clinical care in underrepresented minorities, Claassen and colleagues noted. These issues are germane to Huntington’s disease as the history of clinical treatment “includes eugenics, forced sterilization, and patient stigmatization,” they wrote.
Claassen and co-authors studied patients in Enroll-HD, a registry of more than 20,000 patients from Huntington’s disease centers mostly in Europe and North America. They evaluated differences in baseline performance on functional capacity (activities of daily living), cognitive tasks, motor function, and psychiatric well-being, as well as medical management of chorea. How functional, cognitive, and motor scores varied over time was also assessed.
The researchers used propensity score matching for age and CAG-age product (CAP) scores to account for disease burden. The analysis included people whose gene expansion was pre-manifest or manifest for Huntington’s disease.
The matched cohort consisted of 208 white, 104 Black, 208 Hispanic, and 104 Asian participants. Most Black participants were from North America. In each group, about 50% to 60% of participants were women. Black participants had the highest percentage of high school graduates and beyond (96%).
More than a quarter (28.8%) of Black participants were on chorea medications, which was significantly higher than white (9.96%), Hispanic (14.9%), or Asian (7.6%) participants (P<0.01).
Compared with other groups, Black participants had lower total functional capacity scores. They also had a lower processing speed and visual attention scores, and lower cognitive performance, compared with white and Asian participants.
Total motor scores on the Unified Huntington’s Disease Rating Scale were worse for Black participants than white, Asian, or Hispanic participants at baseline. There were no differences in psychiatric symptoms between races.
Overall, the largest effect sizes were found between Black and white participants on baseline cognitive and motor scores. The trajectories of cognitive, functional, and motor function measures over time were similar between groups.
The findings suggest there may be a large cohort of Black patients not evaluated at Huntington’s disease centers, the researchers noted.
“While Huntington’s is a rare disease, it is a microcosm of neurodegenerative disease in the United States,” Claassen said. “A comprehensive change to our care model will allow us to improve the identification, treatment, and monitoring of patients who suffer from neurodegenerative diseases.”
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
This study had no funding.
Researchers declared no competing interests.
Primary Source
Movement Disorders
Source Reference: Buchanan DA, et al “Racial differences in the presentation and progression of Huntington’s disease” Mov Disord 2023; DOI: 10.1002/mds.29536.
Please enable JavaScript to view the