An experimental treatment that delivers an electrical current to the spinal cord appeared to notably improve the ability of a man with Parkinson’s to keep his balance and walk without freezing up, a development that experts say could be a dramatic advance if it is found to deliver similar benefits in larger studies.
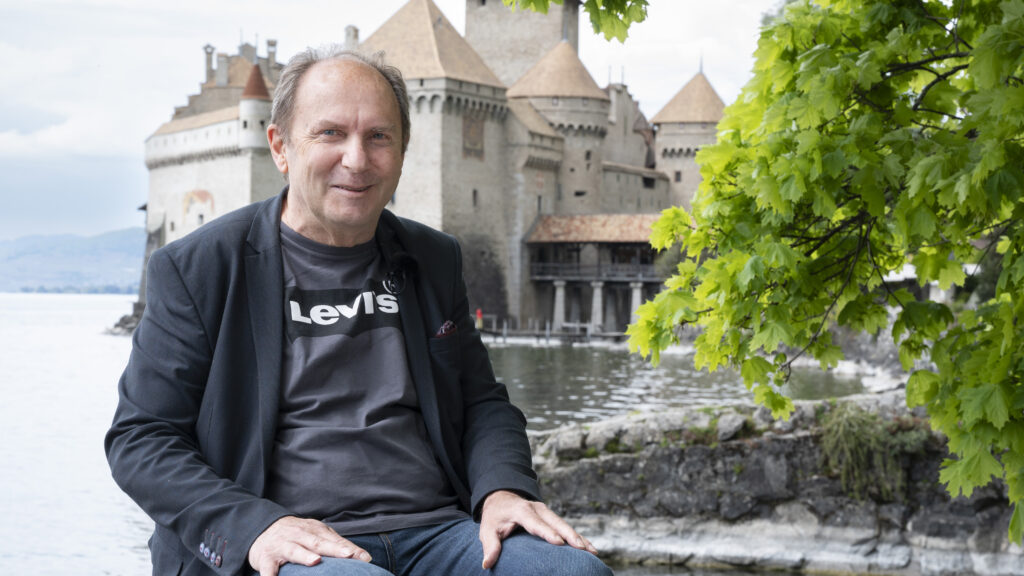
The volunteer, identified as Marc, a 62-year-old who has had Parkinson’s for 30 years, spoke on a call with reporters last week. He said that before the neurostimulation device was installed, he would fall five or six times a day. He was forced to stay home and to stop working. Now, he said, he can go out alone again without terrifying his wife, or even walk inside a store, something he couldn’t do before.
advertisement
Marc has also taken medicine for Parkinson’s and undergone a treatment called deep brain stimulation. The benefits of the treatments appeared to be additive. Marc spoke in French, and his comments were translated by study researchers.
“I really believe that these results open realistic perspectives to develop a treatment that alleviates gait deficits due to Parkinson’s disease,” said Jocelyne Bloch, a neurosurgeon at CHUV Lausanne University Hospital in Lausanne, Switzerland, who was a senior author of the research, which was published Monday in Nature Medicine, a peer-reviewed journal.
Outside experts were enthusiastic about the results, but both they and the study authors emphasized that much larger studies, perhaps including a placebo control, would be needed before such a treatment could be made available widely.
advertisement
In an opinion piece published alongside the study, researchers Aviv Mizrahi-Kliger and Karunesh Ganguly, both from the University of California, San Francisco, called the work “an impressive tour-de-force study.” They wrote: “It will be exciting to see how this approach translates to a larger group of patients with freezing-of-gait in the setting” of advanced Parkinson’s disease.
The study also included results from trials in primates that had a genetic disorder similar to Parkinson’s.
It’s believed that one reason people with Parkinson’s lose control of their bodies is because signals to and from the brain are no longer strong enough to be heard. Providing the correct amount of electrical stimulation to nerves, the theory goes, ensures the reduced signals that are still being sent along nerve fibers are “loud” enough that communication can be restored.
But turning that theory into practice has been anything but easy. Past versions of spinal cord stimulation have been touted as having produced dramatic improvement in patients, but subsequent studies in larger patient groups did not show good results, said Mark Hallett, a distinguished investigator emeritus at National Institute of Neurological Disorders and Stroke, part of the National Institutes of Health.
What’s different from previous attempts with the current work is that the technology stimulated the six major nerves entering the spinal cord in a pattern that corresponded to the timing of activation of motor neurons that are active when someone walks. In the studies of non-human primates, the technology was linked to animals’ brains, but that wasn’t possible in Marc’s case because of the deep brain stimulator already implanted in him. In his case, the device, called a neuroprosthetic, detected what he was trying to do from movements in his legs. The device required considerable fine-tuning before it was able to help him move, and it does require a surgery to be implanted.
“This is certainly a clever approach, but more patient data are needed, and there is the typical concern that patients with Parkinson’s disease are very placebo responsive,” Hallet said.
On the call with reporters, both Bloch and Marc himself said that they couldn’t imagine the effect was the result of a placebo effect.
“I have to say that even with him, we’ve tested different amplitudes. We keep asking for feedback from him about, well, how much of this could be, you know, you mentioned placebo. I mean, during all our evaluations, we don’t tell him how we’re stimulating,” said Eduardo Martin Moraud, another study co-author. “And so we try as much as we can to be blinded.”
Beyond the possibility of a placebo effect, outside experts also raised concerns that the impact of the disease can be variable and that different people can respond very differently to a treatment, concerns the researchers acknowledged.
The work was spearheaded by Grégoire Courtine, a professor of spinal cord repair at the Swiss Federal Institute of Technology in Lausanne. For two decades he has been working on using electrical stimulation to improve the functioning of people who have suffered paralysis from spinal cord injury. In some cases, such technology has allowed people with paraplegia to move from wheelchairs to using walkers.
Courtine and Bloch have co-founded a company, Onward Medical, based in the Netherlands, that is working to commercialize this work. Onward has raised a total of $168 million, according to PitchBook, but in the current biotech and medical device downturn has a market capitalization of $100 million. The company could benefit from the development of the technology in Parkinson’s, too.
Courtine said that in larger trials the Food and Drug Administration would at least want to discuss using a placebo or sham control, and could require one. He said that there are current discussions for using one of his devices that is being tested to treat low blood pressure due to spinal cord injury. He said that he hopes the FDA may be becoming more willing to not include a sham control arm in future studies, given the difficulty of doing so. A patient can feel the input from the device, making it difficult to blind treatment. “So we’ll see,” he said. “It’s unclear whether we will do this in the future.”
The next step will be to try implanting the device in six more volunteers with Parkinson’s disease, something that Courtine said will happen over the next year or so. The work is being funded by the Michael J. Fox Foundation as part of a grant of more than $1 million.
Catherine Kopil, MJFF’s senior vice president of clinical research, said that her team is “energized” by the potential of the research, especially given the promise seen in patients with spinal cord injury. But she, too, emphasized that much larger studies will need to be conducted.
“More work is needed to inform the design of a large-scale clinical trial to establish its safety and efficacy to alleviate gait deficits and reduce the occurrence of freezing-of-gait,” she said.
The result is in some ways analogous to early results emerging in cell and gene therapy, said Vikram Khurana, the chief of the division of movement disorders at Brigham and Women’s Hospital and a neurology professor at Harvard.
Such an “n-of-1” study — a study of a single patient — can have implications not only for developing a therapy but for understanding the biological processes behind a disease.
But a result from a single patient using a complex technology brings two challenges, he said. First: “How applicable is one person’s finding to a population?” Second: “How can one truly make boutique treatments accessible to a large number of patients, and affordable?” He notes that spinal stimulation is “nontrivial to optimize and expensive.”
“The idea is really after this first phase to launch a large-scale pivotal trial to really validate the safety and efficacy of the therapy and make it available for the people who need it,” said Courtine. “Of course, it’s not tomorrow. We’re talking about at least five years of development and tests. But we are certainly committed, with Onward Medical, to achieve this next step.”
Correction: A previous version of this story misstated the amount of the Michael J. Fox Foundation grant.