Tarek Loubani looked around at his fellow doctors at Al Shifa Hospital in Gaza City and realized he held one of just two stethoscopes in the room.
It was 2012, and he was treating patients injured during the recent clashes between Israel and Palestinian groups. Without stethoscopes, providers knelt down to patients’ chests to check if they were breathing. Loubani, an emergency room physician in Canada and Kuwait-born Palestinian refugee who regularly works in Gaza, wondered how health care workers could manage without one of medicine’s most basic tools; a cornerstone of triaging patients. Even his nephew’s toy plastic stethoscope was preferable.
advertisement
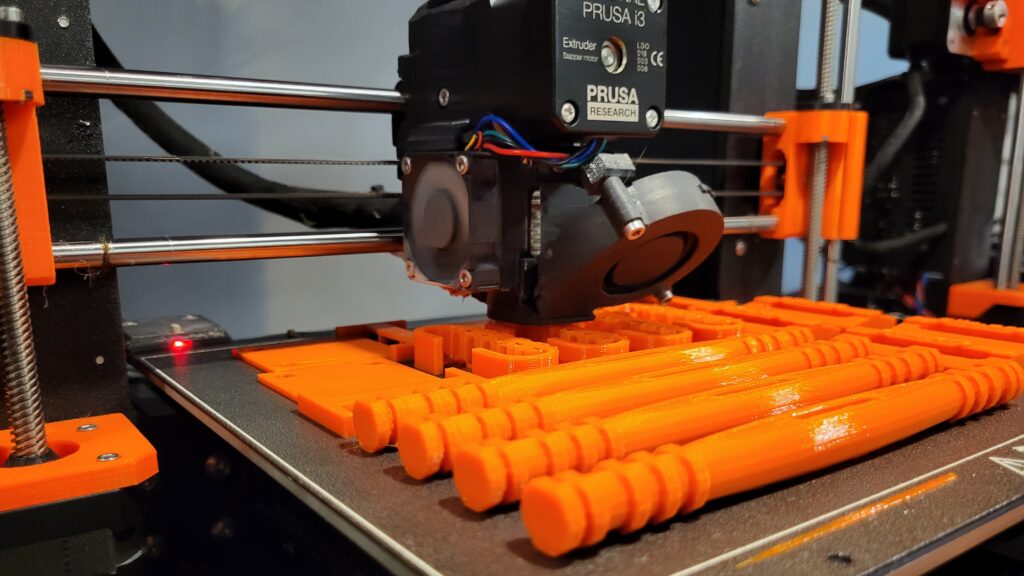
The stethoscope — compared to 3M’s Littman stethoscopes in a validation study — became the inaugural device of the Glia Project, a group founded by Loubani in 2016 that 3D prints open-source medical equipment for low-resource areas. Loubani grew the organization with the help of Carrie Wakem, a former hospital colleague who now serves as Glia’s executive director. The tiny group is pioneering a bold new vision for democratizing medical devices, starting in war-torn areas where they’re most needed.
“It’s not just about developing a 3D-printed stethoscope,” Wakem said. “It’s also about sharing the device design and the code so that other people can replicate what we’re doing.”
Aside from the stethoscope, the around 20-person Glia team manufactures tourniquets, ear otoscopes, and caps to stop bleeding in dialysis patients. They are based in Canada, but also print the devices from offices in the United States, Poland, and Gaza, selling these devices for exactly the price it takes to make them. This means the enterprise runs primarily on grants and donations, creating an often financially precarious situation.
advertisement
“We’re operating like this nonprofit organization that has no money, but we’re doing real research with real universities,” Wakem said. “We’re doing all our own R&D, all our own manufacturing.”
Glia’s focus has returned to Gaza in the midst of a catastrophic conflict between Hamas and Israel. Earlier this month, the militant group killed more than a thousand people in Israel living near the Gaza strip, and took several hundred hostage. Israel has since responded with airstrikes, killing thousands more in Gaza. The government also declared a complete siege of Gaza on top of an existing 16-year blockade, blocking critical supplies from entering the area. United Nations officials are reporting dire shortages in food, water, and fuel. This past weekend, Gazans experienced a total electricity blackout.
The most basic medicines and devices are scarce, leaving doctors scrambling and health systems on the brink of disaster. Glia’s engineers in Gaza are unable to print tourniquets after Israeli air attacks damaged their office, so the team is preparing to transport tourniquets from Canada or Poland when more aid is allowed into Gaza through Egypt.
“The current conditions make it impossible to do our work but as soon as we have a chance we will produce as many [tourniquets] as we can,” Hanan Abu Qassem, administrative director of Glia’s Gaza office, told STAT.
Glia is not able to produce tourniquets on a large scale, but even a hundred makes a difference, Wakem said.
“There are a lot of medical aid people that know the basic necessities,” Wakem said. “What Glia is doing is very specific.”
A partnership with large medical device manufacturers could dramatically increase the scale of Glia’s operation, but Wakem said the team isn’t interested. Nor is the team interested in simply donating their products to communities in need. The goal is to empower local groups who are able to 3D print devices themselves. Eventually Glia wants to create open-source pulse oximeters and electrocardiograms.
“Glia isn’t interested in mass production,” Wakem said. “That’s not our model. Our model is to help other people figure out how to get exactly what they need, and exactly how they need it.”
Gaza isn’t Glia’s only target area. The team mobilized in Ukraine after Russia’s 2022 invasion, and they’re looking to sell tourniquets to more public centers in the U.S. in light of waves of mass shootings — most recently in Maine this past week.
But Gaza remains a hub for Glia, given the area’s severe lack of medical devices historically, not only during active war. After Hamas took over Gaza in 2007, Israel clamped down on movement of people and goods in order to defend itself. The government listed a variety of items as “dual-use,” meaning they could potentially be used to develop weapons in addition to their normal applications. The list includes a range of imaging machines. STAT reached out to an Israeli government spokesperson for comment on the blockade but did not hear back.
“Medical devices have been among the most consistently restricted, especially devices used for X-rays, PET scanners, CT scanners,” said Yara Asi, a professor in global health at the University of Central Florida. “Israel almost has a blanket ban on those because of the radioactive material and by their argument the potential for those materials to be reused.”
Asi, who was born in the West Bank and whose research centers on vulnerable populations, said people with complex medical conditions in Gaza and the West Bank will frequently forgo doctor visits. There’s a “why bother” sentiment, Asi said, because it’s so difficult to access diagnostic care. It’s a stark contrast from Israel, one of the healthiest countries in the world as well as a center of biomedical innovation.
“What we see is that many cancers and other chronic ailments in Gaza are diagnosed at much later stages,” Asi said. “There’s very little preventive care in the occupied territories. People aren’t getting regular checkups and preventive bloodwork and diagnostics.”
Well-meaning donors have sent equipment like scanners and dialysis machines over the years, but if they break, it’s almost impossible for Gazans to acquire replacement parts. The result is a graveyard of medical devices, Wakem said; junk that simply takes up space. Glia received a grant through Western University in Ontario to inventory and repair the machines in Gaza, which they plan to focus on when the violence dies down.
In Gaza, devices are frankly the least of doctors’ many concerns right now. Surgeons are operating on patients without anesthesia, and using vinegar instead of antiseptic. But Asi emphasized that Glia still has a role to play, especially as a model for aid organizations trying to create lasting, self-sufficient health systems.
“If we genuinely want to help them, we don’t want to impose what we think that they need,” Asi said. “Initiatives like the Glia Project differentiate themselves because they saw a need that was already there and they tried to find a way to fix it by working with local communities.”