When my wife, Laurie, completed her ninth in vitro fertilization cycle in the spring of 2000, we had more than 150 fertilized embryos in frozen storage at the Center for Reproductive Medicine and Infertility at the NewYork Presbyterian Hospital-Weill Medical College of Cornell University.
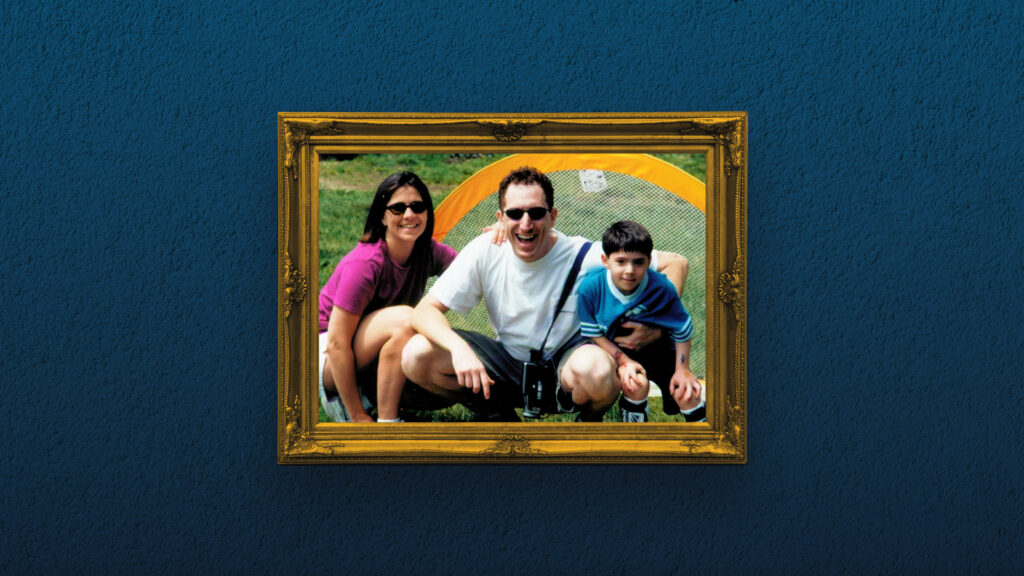
We were not stockpiling them for later use. At the time, our son Henry was 5. At birth, he had been diagnosed with a fatal genetic disease, Fanconi anemia. We were using IVF together with preimplantation genetic diagnosis (PGD) in hopes of having a healthy baby who could also save Henry’s life with a cord blood transplant.
advertisement
PGD allows screening of embryos for genetic diseases like Fanconi before implantation. It has given families like ours a chance to have healthy children while avoiding abortion. We were planning on having additional kids, but as carriers of a fatal disease, each natural pregnancy was fraught with a possible death sentence for the baby. As the Alabama Supreme Court now declares frozen embryos to be children, legislators debating “personhood” must remember the real lives not only conceived but also saved by IVF.
Fanconi anemia causes bone marrow failure, organ defects, and cancer susceptibility. When Henry was born, doctors told us that the chance of his survival without the right HLA matched transplant, the right combination of leukocyte antigen proteins, stood at 18%. With a perfectly matched sibling transplant, they said, Henry’s chances to live rose to more than 85%.
Over the course of less than three years, Laurie endured 353 painful injections and procedures in nine IVF attempts, while doctors monitored Henry’s declining health. Our goal was to implant only embryos that were both disease-free and a genetic match for Henry. Laurie did not get pregnant with the few embryos that eventually were implanted. In a perverse twist of fate, the most viable embryos Laurie produced had the disease, and they were not implanted but instead donated to research both to better understand Fanconi anemia and to improve PGD for families that followed us.
advertisement
I understand that there are ethical issues surrounding use of IVF paired with PGD. Not all families are comfortable with creating embryos in the laboratory knowing that some of them will not be implanted. And no one would advocate creating a child only to save another’s life. But the choice of whether to employ screening is a deeply personal one and should be considered with great care by families in consultation with their doctors and genetic counselors.
Henry’s health worsened, so we had to go to transplant without a matched sibling. The statistics proved accurate. After transplant from an unrelated donor, Henry spent two agonizing years in and out of hospitals before passing away in 2002 at age 7. As we were ending our IVF attempts, another Fanconi family began down the same path. They contacted us hoping to work with our medical team. On their third try with our doctors, Sharon Harari and Yavin Atzmon conceived Alma, whose umbilical cord blood saved her brother Amitai’s life.
In 2022, Mark Hughes, the pioneer of PGD for HLA matching and Henry’s doctor, said on a podcast that these techniques have allowed thousands of children to save their siblings’ lives through cord blood transplant, a procedure that uses hematopoietic stem cells drawn from the umbilical cord after it is removed from a newborn. The umbilical cord is normally disposed of as medical waste. But in PGD, stem cells collected from cord blood can rebuild diseased bone marrow in disorders like Fanconi anemia. The fruits of PGD are living children, saved lives, and intact families.
After almost 22 years without Henry, our family still feels his absence deeply. In addition to continuing to process our own grief, my wife and I work hard to support Henry’s surviving siblings, who have had their own ongoing challenges coping without their beloved brother. For families inheriting fatal illnesses, PGD offers hope of life and healthy families. As Alabama and other states consider embryos’ legal status, the true impact of IVF and PGD on families must not be forgotten.
Last month, 25-year-old Amitai and I shared a dinner together. We spoke of his health, his studies to become an EMT, and his medical school aspirations. As we parted, he nervously asked if his existence pained Laurie and me. I assured Amitai that, to the contrary, he epitomizes the joy and life that IVF with PGD makes possible. As legislators in Alabama and elsewhere decide how to move forward, they must listen to the voices of families relying on PGD to prevent disease, stave off almost certain death, and save lives.
Allen Goldberg is a communications and public affairs professional in Washington, D.C. He serves on the Board of the Hope for Henry Foundation, leveraging behavioral science to improve medical adherence and outcomes for hospitalized children across the United States.