Research led by the University of Pennsylvania has discovered that a viral method of entering cells can be harnessed to get therapeutic CRISPR-Cas gene editing complexes into cells more easily.
Writing in the journal Nature Biotechnology, the investigators report that their new system —Peptide-Assisted Genome Editing (PAGE)—allows quick and effective editing of cells with limited toxicity.
They believe the new system could revolutionize advanced cell and gene therapies involving gene editing where getting the editing machinery into cells is currently a limiting step.
“Current methods of getting CRISPR-Cas systems into cells, which include the use of carrier viruses and electric pulses, are inefficient for cells taken directly from patients (called primary cells). These methods also typically kill many of the cells they are used on, and can even cause broad unwanted changes in gene activity,” said co-senior author Shelley Berger, the Daniel S. Och University Professor in Cell and Developmental Biology and Genetics and director of the Penn Epigenetics Institute, in a press statement.
One of the most advanced and successful combined cell and gene therapies, chimeric antigen (CAR) T cells, have revolutionized oncology. To get to the next generation of these therapies effective CRISPR-based gene editing tools are required.
“Currently, however, efficient delivery of the CRISPR system into primary T cells remains a major challenge, relying heavily on optimizing the use of viral vectors, physical electroporation and/or lipid nanoparticles individually or in combination,” write the researchers.
“Related challenges exist in mouse disease models, where the difficulty of Cas protein delivery via viral vectors or other approaches often necessitates a cumbersome and lengthy process of breeding Cas9-expressing transgenic animals to different inducible or lineage-specific strains for genetic studies in vivo.”
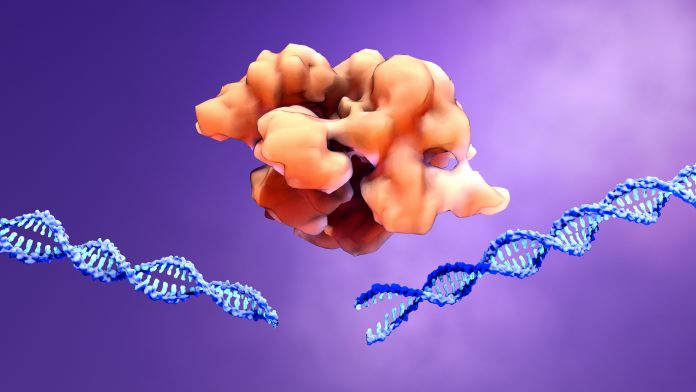
In this study, the researchers assessed whether PAGE could be the answer to these problems. The system includes a CRISPR-Cas protein such as Cas9 or Cas12a and also a cell-penetrating ‘endosomal escape’ peptide that allows delivery of the editing machinery.
The peptide they used to help enter target cells is a fusion peptide called TAT-HA2 derived from the HIV and influenza A viruses combining the ability to penetrate cells and use a process known as endosomal escape.
The team tested PAGE in a mouse model and in human cell lines and showed editing efficiencies of 98% and higher for T cells and hematopoietic stem and progenitor cells. The system is also fast with an incubation period of only 30 minutes. So far it appears to have low cellular toxicity and limited transcriptional disruption.
However, “the potential for pre-existing immunity against components of the PAGE system may limit its use for in vivo delivery but is relatively less of a concern for ex vivo gene editing,” write the authors. Who add that “further research is needed to fully evaluate the immunogenicity of the CRISPR-PAGE system in primary cells.”
