A live, wriggling parasitic roundworm, 80 mm long, was extracted from the brain of a 64-year-old woman in Australia.
The worm was a third-stage larval form of Ophidascaris robertsi and was surgically removed from the patient’s right frontal lobe, reported Sanjaya Senanayake, MBBS, of the Canberra Hospital in Australia, and co-authors in Emerging Infectious Diseases.
The helminth typically is found in carpet pythons. “This is the first-ever human case of Ophidascaris to be described in the world,” Senanayake said in statement.
Larvae from the roundworm usually are found in small mammals and marsupials that are eaten by the python, allowing the life cycle to complete itself in the snake, Senanayake explained.
O. robertsi nematodes are native to Australia, where adult worms inhabit a carpet python’s esophagus and stomach and shed eggs in the python’s feces.
Despite no direct snake contact, the patient often collected vegetation from a nearby lake area to use in cooking. The patient likely contracted the parasite from touching or consuming native warrigal greens contaminated with python fecal matter, the researchers noted.
“We hypothesized that she inadvertently consumed O. robertsi eggs either directly from the vegetation or indirectly by contamination of her hands or kitchen equipment,” they wrote.
The patient’s symptoms first started in January 2021. She developed abdominal pain and diarrhea, followed by dry cough and night sweats. No parasites were identified in blood, or respiratory or lung biopsy specimens.
The patient was diagnosed with eosinophilic pneumonia of unclear etiology. She began taking prednisolone 25 mg daily with partial symptomatic improvement. Three weeks later, she was admitted to a tertiary hospital with recurrent fever and persistent cough. Bacterial, fungal, and mycobacterial cultures were negative.
Findings suggested T-cell-driven hypereosinophilic syndrome; the patient began treatment with prednisolone 50 mg daily and mycophenolate 1 g twice daily. Because of her travel history, the possibility of false-negative parasite serology, and increased immunosuppression, she also received ivermectin 200 μg/kg orally for 2 days and a repeat dose after 14 days.
In January 2022, her physicians added mepolizumab 300 mg every 4 weeks because they could not lower her prednisolone below 20 mg daily without a flare in respiratory symptoms.
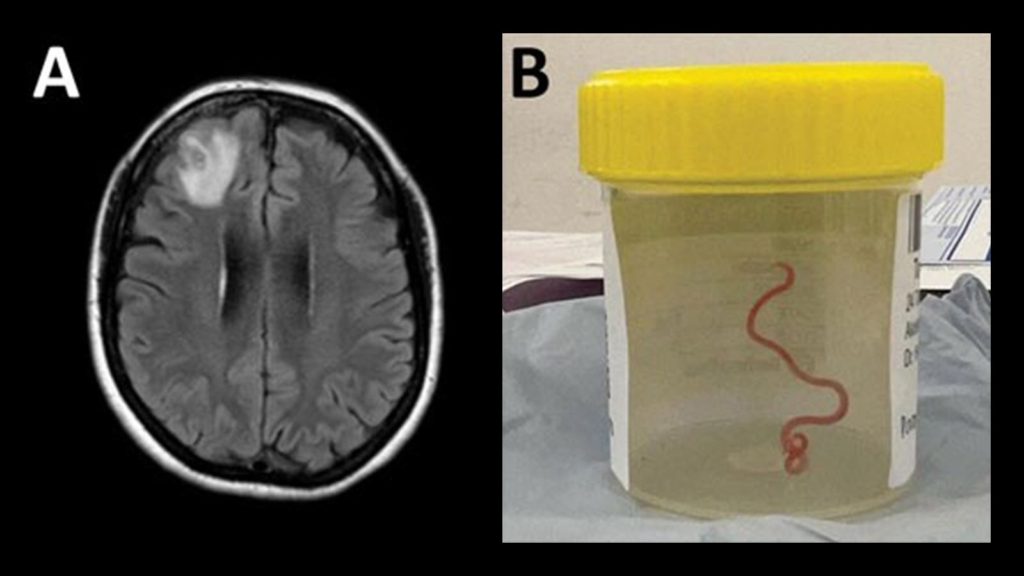
Over 3 months in 2022, the patient experienced forgetfulness and worsening depression while continuing prednisolone 7.5 mg, mycophenolate, and mepolizumab. Brain MRI at that time showed a right frontal lobe lesion.
An open biopsy revealed a string-like structure within the lesion, which was removed and identified as a live, motile roundworm, 80 mm long and 1 mm in diameter. Neurosurgeons performed a circumferential durotomy and corticotomy and found no other worms.
After the helminth was removed from her brain, the patient received 2 days of ivermectin, 4 weeks of albendazole, and a weaning course of dexamethasone. Six months after surgery, her peripheral blood eosinophil count remained normal. Neuropsychiatric symptoms persisted, but improved. The patient continues to be monitored.
Ophidascaris infection does not transmit between people, Senanayake noted. “However, the snake and parasite are found in other parts of the world, so it is likely that other cases will be recognized in coming years in other countries,” he said.
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
The researchers reported no disclosures.
Primary Source
Emerging Infectious Diseases
Source Reference: Hossain ME, et al “Human neural larva migrans caused by Ophidascaris robertsi ascarid” Emerg Infect Dis 2023; DOI: 10.3201/eid2909.230351.
Please enable JavaScript to view the