For years, researchers have been hopeful they could get under the hood of multiple sclerosis. The neurological condition shows up in over 2.5 million people around the world, but it doesn’t always look the same. If science could point its light in just the right way, patients might be sorted into disease subgroups, and treated more successfully depending on their kind of MS.
A new study out of Germany gives it a shot, offering up three MS subtypes based on immune markers found in patients’ blood — each group with slightly different disease progression.
advertisement
The MS connection of the senior author, Heinz Wiendl, could start in his home. His mother had the condition. But that’s not really it, he says. He was always fascinated by immunology and neurology, and how MS went from an untreatable disease to a known, druggable condition in less than 40 years.
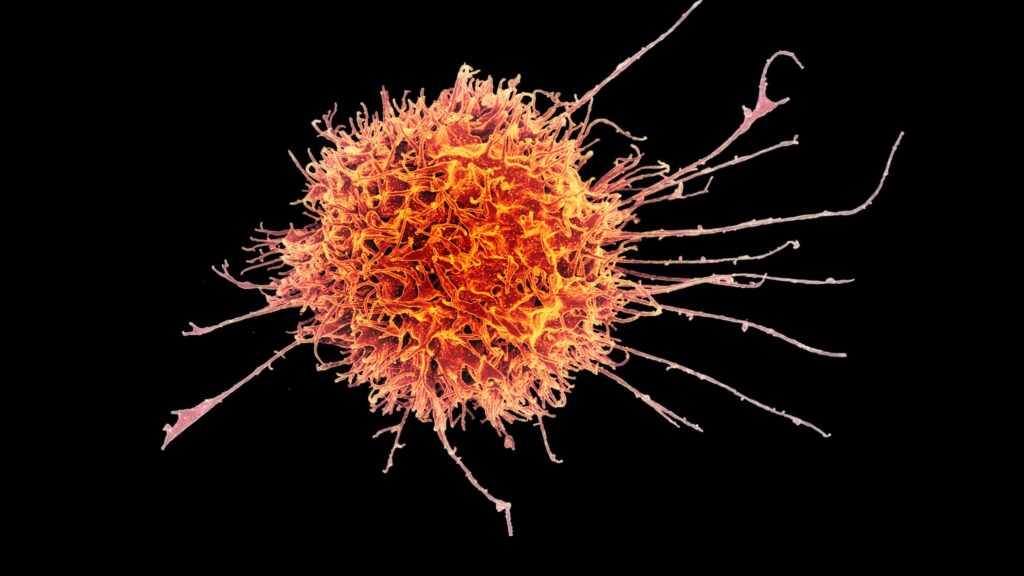
He’s been in the field for more than half of that time, trying to get a grasp on how the immune system fusses and frays in response to antigens, and how that turns into a difficult chronic condition. MS causes vision problems, fatigue, and weakness or spasms in the arms and legs, among a host of other symptoms. The condition is thought to be more common in women.
Most recently, Wiendl set out to prove a hypothesis he’s been building for years: that MS patients have immunological signatures in their blood that match certain versions of the same disease.
advertisement
With collaborators at a half dozen institutions across Germany, Wiendl, a professor of neurology at the University of Münster, launched a multi-center cohort study of 500 patients with early-stage MS. Those newly sick people were a right fit because the “immunological derailment has happened, but it’s not yet spread out and diverged,” he said. Plus, patients hadn’t undergone treatments that changed their immune systems.
And Wiendl, with all his years of research, tried to wipe his mind clean of all presuppositions he had about the disease and go in agnostic. The team assessed the quantity and quality of various immune cell populations, not favoring any in particular. And then they let an algorithm determine whether certain cell populations, or a combination of them, were more prevalent in these MS patients.
It’s a little like Lebron James, Wiendl said. If the cameraman is only ever focused on James, the audience will miss what the other players are doing. Sure, the superstar — or highly suspect immune cell — is captivating, but viewers could miss important plays elsewhere on the court.
“If Lebron James in the end happens to make the most goals or baskets, we will find out anyway. But we have not overlooked the others,” he said. This is the “unsupervised” approach the team used.
In the end, there was some superstar-watching: The researchers confirmed that players other researchers had spotted in MS were playing a role in their cohorts, too. But they also found new things, published Wednesday in Science Translational Medicine.
Most notably, Wiendl and his collaborators say they found unique stamps of immunological activation that correspond to specific subgroups, or endophenotypes. And each subgroup — identified as E1, E2, and E3 — had its own disease trajectory when they followed patients for four years.
E1 patients had alterations in the CD4 T cell compartment, the helper cells that can activate other immune cells, and inflammatory proteins that have been associated with autoimmune disease. This group was associated with earlier structural brain damage, greater disease severity, and higher disability — their condition was “much worse from the beginning,” Wiendl said.
Meanwhile, E2 had differences in natural killer cells, which take down sick cells. And E3 patients had changes to highly toxic CD8 T cells, making it a more “inflammatory” category. E3 patients had a higher relapse rate within the first year, and more MS lesions that point to issues in the blood-brain barrier. Researchers also found more immune cells in the cerebrospinal fluid of E3 patients (this data was available for about 170 of the patients).
There was some overlap, but Wiendl and his colleagues believe the subtypes are distinct and could help predict how patients’ disease progresses. They don’t know exactly how stable the subtypes are over longer periods of time, or if treatment changes it. But Wiendl said cellular signatures were found over time in the handful of patients who went untreated, “including up to nine years within one individual,” the authors note in the study.
These differing subgroups could suggest the disease arises through a multitude of immune system pathways. Not only that, Wiendl said, but the groups responded differently to treatments over time — potentially a valuable insight for drug developers and clinicians.
For example, the inflammatory E3 group for the most part didn’t respond to treatment with interferons, commonly used disease-modifying therapies first approved for MS in 1993. But these patients did improve by taking monoclonal antibodies, such as alemtuzumab (Sanofi Genzyme’s Lemtrada) and ocrelizumab (Genentech’s Ocrevus).
The ability of the endophenotypes to predict a patient’s future condition needs to be checked by other researchers, and in a different population, said Alberto Ascherio, who led a pivotal study linking MS to previous Epstein-Barr infection and was not involved in the German study. He called the new study “interesting” for those in the field and said that endophenotypes could, in theory, help to personalize treatment.
But the science isn’t there yet, Ascherio added. Personalized medicine in MS is still a “fashionable word that is more a marketing pitch than a reality.”
Wiendl said he hopes other researchers can use the study’s data to test and confirm how well different MS treatments work for patients with these immune signatures, and to find other potential therapies. Wiendl also programmed an app with the data, and said he is developing a test to help others discriminate between the E subgroups. His spinoff company has patented the endophenotypes.
Ideally, one day there will be a simple test to classify patients and help doctors find the most effective treatment, Wiendl said.
“We really want to transform patient care and not just open the door,” he said.
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.