Over the past year, I have watched many children die of measles.
In the final stages, little lungs, filled with fluid and racked with inflammation, struggle for oxygen. The victims breathe faster and faster, gasping for air until, exhausted, they stop.
advertisement
Where I live, in one of the poorest places on earth, measles kills thousands of children a year. It’s a grim lesson about a disease that should have been eradicated years ago. And it’s a grave warning against assuming “it can’t happen here” in more fortunate countries like the U.S., where the disease is making a comeback as parents fail to take the disease seriously. For years, U.S. pediatricians have gone their entire careers without seeing a case of measles, much less a death. Now, I fear, that may change.
I’m chief of medical research — and the only pediatrician — for Sankuru Province in the Democratic Republic of the Congo. Sankuru is about the size of Ohio and has around 3 million people, half of whom are under 18. The Congo’s poorest province, it is profoundly underdeveloped. It has no paved roads or airports. Most villages can be reached only on foot or by using tiny motorcycles, which few can afford. Municipal water or electrical systems do not exist. I came to Sankuru for a unique reason: I grew up there. My family has been serving in Sankuru since 1950. Since I was a child, working alongside my mother in under-5 baby clinics, I have felt a call to serve the children of Sankuru.
Last year, we had one of our periodic measles epidemics. According to our limited “official” data, there were almost 21,000 cases and more than 500 deaths, mostly very young children. A better estimate would be multiplying those numbers by at least four.
advertisement
I watched helplessly at one hospital, roughly the size of a small house, as the overwhelmed staff turned away about 100 sick children a day. In the U.S., children would be given oxygen and put on respirators. That doesn’t happen in Sankuru. There are no respirators, no bottles of oxygen, and often, not even IV fluids for a dehydrated kid. (Infants struggling to breathe with measles often don’t have the energy to nurse.) The children are sent home to get better — or to die. Fortunately, many do get better. But everyone knows friends who have lost children to measles.
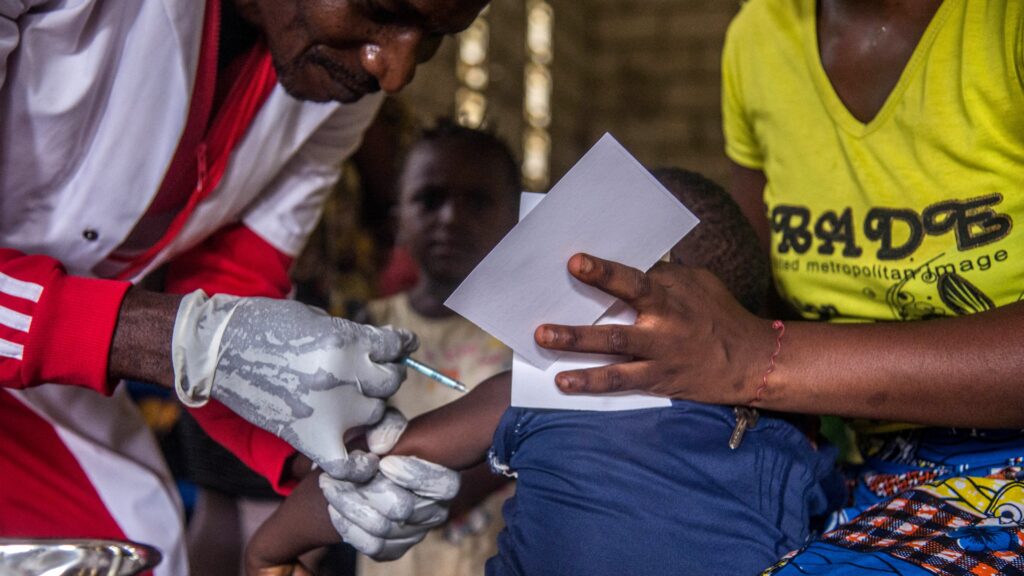
To be sure, Sankuru is not the U.S., where vaccines are plentiful and medical resources can blunt the impact of measles. In Sankuru, we struggle to immunize children. Lack of funding and primitive infrastructure make it very difficult to get vaccinations to kids. We’re lucky to have vaccinated even 20% of children for measles. I’ve never met a mom there who turned down the shots for her kids.
I decided to tell this story after the measles outbreak in Florida, so that parents would know what a miracle vaccines are. The point is not to say that measles will kill your children in America, because it probably won’t. The point is that it can make them — and many other children — very, very sick. Why would parents do that when the safe alternative is readily available?
In the Sankuru, we’re reduced to waiting for the epidemic to burn itself out, having no more victims to infect. And, indeed, after a measles epidemic like the last one, survivors of the disease are immune. But 125,000 babies are born in Sankuru every year — a new, susceptible group of kids. In a couple of years, without better access to vaccines, many of them will die as the agent of death returns for fresh victims.
Child mortality is a bitter fact here. The mortality rate for Sankuru children under 5 is 15% to 20% — no one knows the exact number because the data collection is as poor as the population. (By comparison, the under-5 mortality rate in the U.S. is less than 1% — 6.2 deaths per 1,000 live births in 2021.)
I believe the path for children of Sankuru is better preventive health care supported by accurate data systems. With better tracking systems, we can know which kids are immunized — and which aren’t.
But that’s a more arduous journey than traveling the province’s rutted paths. I have an M.D., a masters in public health, a masters in informatics (the science of processing data), and a pediatric residency, all from Johns Hopkins. But in Sankuru, computer skills (and even computers) are hard to find.
Of course, the public health answer to measles is universal vaccination. If there were no cases of this highly contagious disease, there would be no more measles. So, places like Sankuru remain dangerous “hot spots” from which the disease could spread. Other diseases that are rare in the U.S., like polio, are still claiming victims. Malaria is a significant killer.
In the end, the biggest killer of all is poverty. There are too few physicians. Health care workers are woefully underpaid. (My own position is essentially voluntary.) In Sankuru, where the average month family income is equivalent to $100, children frequently die because their parents can’t afford medical care that costs what U.S. families would spend on a restaurant meal.
In measles and money, we often forget how fortunate we are.
Paul Law, M.D., MPH, M.S., is an American physician who, before coming to Sankuru, had a distinguished career in health information systems.