The Office of the National Coordinator for Health Information Technology was born two decades ago, tasked with creating an interoperable health IT infrastructure and shifting the country away from paper medical records.
Much has changed since then. The vast majority of hospitals and physicians now use electronic health records. Nationwide health data exchange under the Trusted Exchange Framework and Common Agreement, or TEFCA, went live in December, after years of work.
And now, artificial intelligence-enabled tools — including products that aim to cut down on providers’ administrative tasks — signal more change ahead for the industry. Late last year, the ONC finalized a sweeping rule that included transparency requirements for certified clinical decision support and predictive tools.
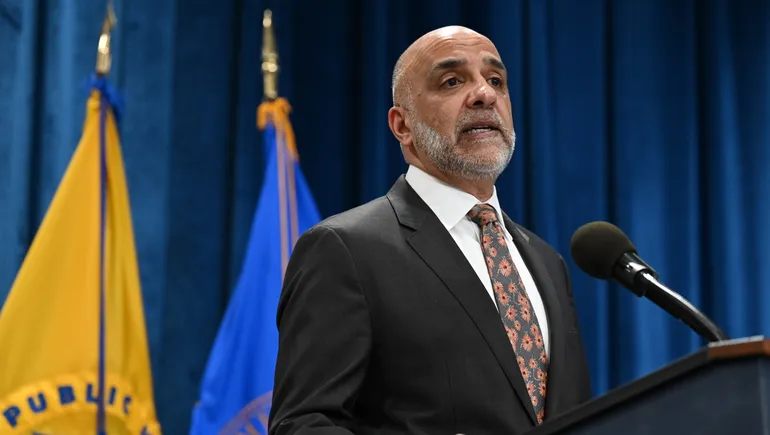
Micky Tripathi, head of the ONC, sat down with Healthcare Dive to discuss the past 20 years and how the agency’s work aims to create the foundation for the next generation of healthcare technology.
Editor’s note: This interview was edited for clarity and length.
HEALTHCARE DIVE: When you look back at 20 years of ONC, what do you see as some of the agency’s biggest accomplishments?
MICKY TRIPATHI: The transformation that the healthcare delivery system, particularly hospitals and physician offices, have gone through in being largely paper-based to what I would argue is starting to closely approximate digital native. It’s pretty hard for any of us to find a paper record on ourselves. I don’t think there are many being recorded.
I think we’ve played a significant role, obviously working in partnership with our colleagues at the CMS, who did a lot to create the incentive structure for providers to adopt electronic health records. And then we certified those systems to be able to create sort of a digital floor or digital foundation on which we can now start to build the 21st century digital healthcare system that all of us are eagerly anticipating.
What are some of your next big goals and priorities for ONC?
We want to continue to fill in the gaps. We’re certainly not pretending that the entire system is digital. There are large parts that didn’t get the benefit of those incentive programs and associated ONC support, like long-term, post-acute care, behavioral health. We didn’t even include human services and social services, which are a very important part of people’s overall health status, even though they’re not what we think of as healthcare in the U.S.
But increasingly, it is building on that digital foundation that we’ve all worked so hard to put in place. What are the higher ambitions that we all have for these kinds of technologies? There is an adage out there, which is that we in technology tend to overestimate the benefits that we’re going to get in five years. And we totally underestimate the benefits in 10 years.
And I think that’s true for electronic health records. There was a lot of anticipation that, once these are in place, they’re going to solve all of healthcare. And of course, we saw that it’s very difficult to adopt these systems, and a lot of contribution to what people call clinician burden.
But now as we look ahead to 10 years, we would not be able to have the anticipated benefits that we’re going to get from AI if we didn’t have these electronic health records in place. We would be so far behind at that point. We’d all be struggling to say, “Wow, AI is really cool. Too bad we can’t use it in the U.S.” Or, “Too bad only the Mayo Clinics and the Mass Generals of the world can use it, but not the federally qualified health centers, not the inner city hospitals.”
EHRs are widely used, but providers still have plenty of complaints about usability, the time it takes to document care and the number of alerts they’re managing. These aren’t new challenges, but what do you think ONC’s role will be to ameliorate these issues moving forward?
There’s a bunch of stuff that people blame on the EHR, but are really about piling onto the EHR. This isn’t to say that the providers’ concerns aren’t real. But there’s a lot of stuff that got added onto the EHR, like extra documentation practices and prior authorization and quality measurements. If you add all of those things onto it, then yeah, it’s going to become a very complicated, unwieldy process for some organizations.
So a part of what we required in the 21st Century Cures Act regulation that we put into place on April 5, 2021, requires that all electronic health information be made available in a machine-readable format. And part of that was the hope that technologies are going to come on the scene that are going to be able to process that data and make it usable for people. And then of course, ChatGPT erupts onto the scene.
Now I’m not suggesting you should do this on public ChatGPT, because there are lots of privacy issues. But you do have the technological ability now to literally take those records, run them through ChatGPT or Llama or whichever one is your choice and it will actually give you a synthesis and a summary of what’s in those records, which is pretty phenomenal.
Now, we still have work to do to assure you as a patient that that’s safe to do. It’s not going to make the serious mistakes that could actually cause you harm. And, as I was describing, we have work to do on the privacy side. You need to be assured that when you use a tool like that, you know what you’re getting into. It either does or doesn’t have privacy protections, but you need to be aware of whether it does or doesn’t, so that you can make a choice of whether you’re willing to take that risk.
This is a good segue into AI. There are plenty of concerns that it’s coming too fast, and we’re not really sure how safe it is or how well it works. As the co-chair of the government’s health AI task force, do you think those concerns are warranted?
It is definitely warranted. We, as a department, are concerned. We, as the U.S. government, are concerned. But we also don’t want to lose sight of the opportunity. We’re big AI optimists. And we do believe, on net, that there’s huge opportunities for patients and for the industry at large.
We need to be able to create the avenues to spur innovation in this area, and take best advantage of these great technologies that are coming into place. But we also want to make sure that patients feel protected. The basic mantra is that we want to make sure that these technologies are used for patients, and not on patients.
I think that for the most part, they will see that provider organizations are being judicious in this because they have safety and quality at heart too.
In almost all cases that I’m aware of, AI-enabled tools are being used, but to help to augment physician decision making, not to replace physician decision-making, which I think is what all of us want. We expect that our doctors are going to use the best possible tools available to them to give us the best possible care. And we want to make sure that these tools fall into that category, or the best possible tools that they trust.
But we also recognize that it’s moving really fast and people are going to adopt it really fast. Without any rules of the road, you will get inadvertent and maybe even malicious outcomes that all of us want to prevent.