Shah is a medical student.
As a medical student pursuing surgery, I must balance learning new skills with properly serving patients and ensuring my team can function efficiently in the bustling hospital. With a scarcity of hands-on opportunities, the gap between theory and practice feels insurmountable. However, I am encouraged by the potential for artificial intelligence (AI)-powered tools to transform medical education. Imagine a world where learning extends into a virtual operating room — with a risk-free environment, unlimited practice, and real-time feedback.
This type of innovation isn’t just about filling gaps in knowledge; it signifies a future where every patient benefits from more skilled and confident physicians. Trainees and experienced surgeons alike can practice their craft prior to operating on patients. This will redefine medical practice itself — if we are lifelong learners, and practice makes perfect, imagine if we could improve the quality of our practice and carry it out in a low-stakes environment.
And what about inside a real operating room — is there a role for AI? Before exploring this question, let’s take a look at where the technology stands today in healthcare.
The Growth of AI in Healthcare
With the emergence of ChatGPT in late 2022, AI rapidly entered popular conversation across industries. While the concept of AI technology has been around since the 1950s, it was not broadly available until recently. Already, AI has shown vast promise in medical care. There are a variety of proven and theoretical uses reported by major health systems and within academic literature. These range from completing routine administrative tasks to preventing medical errors, communicating with patients, and assisting in diagnostics.
A variety of studies demonstrate that AI can efficiently compose physician notes, document appointments, and communicate with insurance companies, freeing physicians to spend more time with patients while reducing burnout. Separately, AI has shown promise in educating patients through the creation of accessible online materials. Moreover, the electronic medical record company Epic introduced an AI-based early predictor for sepsis, which reduced the odds of sepsis-related mortality by 44%. Similar models have been created to predict risks for cancers, infections, and allergies. Finally, AI has shown promise in assisting diagnosticians in the fields of radiology, dermatology, cardiology, and pathology.
Future Uses for AI in Treatment and Surgical Administration
Understandably, many remain reluctant to invite AI into the treatment setting. It is difficult to trust this new technology in directly interacting with patients — particularly in the high-stakes operating room. Nonetheless, several studies highlight the potential to improve disease outcomes, patient experiences, and systemic factors when AI is used with appropriate guardrails.
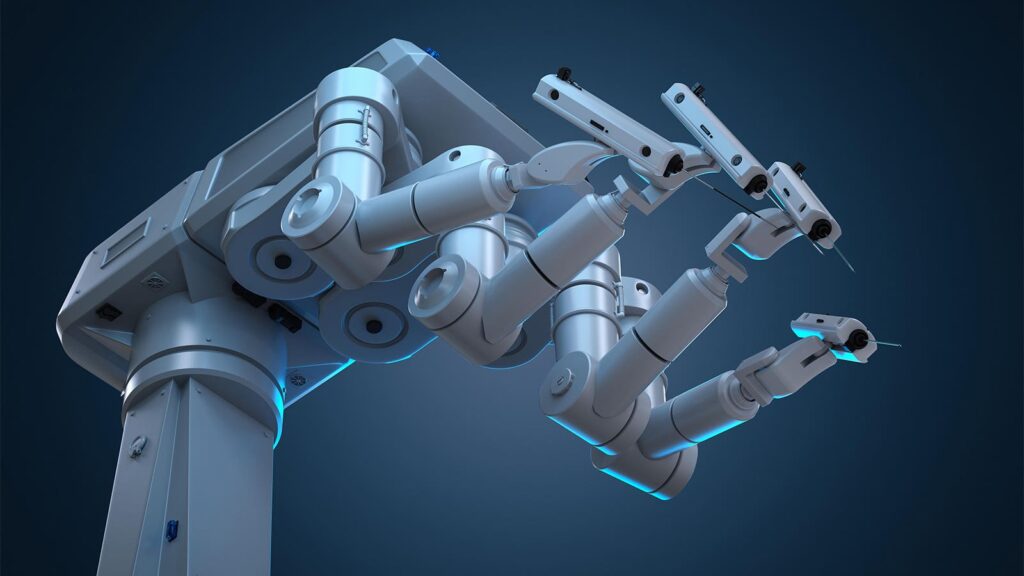
Within surgery, AI holds promise in facilitating robot-assisted procedures, training junior residents, and managing postoperative outcomes. Practice makes perfect, and the best surgeons have learned from decades of fine-tuned skills following countless surgeries. AI also has potential on an exponentially greater scale: to assist decision-making. When a surgeon conducts a video-based procedure, imagine if the AI model could alert them if they were about to make a serious error, much like emergency braking-assist in modern cars. Similarly, the technology could highlight important anatomic landmarks, facilitating the surgeon’s eyes and potentially speeding up the procedure. When it comes to training, residents could practice on realistic AI models before operating on real patients. They could even learn from virtual models based on world-class surgeons’ techniques, allowing the field to pass down its best knowledge to future generations.
Surgery departments have begun using AI to tackle systemic issues that have plagued operations for decades. I’ve seen how common surgical delays are, due to difficulties in calculating operative time, allocating resources, and anticipating intraoperative complications. Patients often wait for weeks or months to receive important elective procedures. Staff are forced to work overtime due to inefficient perioperative processes. AI could help predict surgeries likely to run overtime and help schedulers buffer this cascade. Using AI to assist administration would ultimately benefit patients, who could access care more predictably and efficiently.
Finally, within the electronic medical record, AI has exhibited the ability to analyze a patient’s history, operation, and real-time clinical data to predict postoperative complications and patient needs. This could prevent major issues like infections, bleeds, and the need for reoperation. While physicians and nurses certainly monitor inpatients after their procedure, it’s difficult for any human to identify nuanced changes in vital status or adequately synthesize millions of data points that may be indicative of an impending complication. Moreover, AI could facilitate remote monitoring, allowing for more same-day discharges with safe recovery from the comfort of a patient’s own home.
Limitations of AI in Surgery
Of course, AI comes with limitations. At the end of the day, we must ensure AI remains limited to a decision-support role, while well-trained human physicians are responsible for the final decision. AI should not be used to replace physicians, but instead to facilitate and improve their work. This would ensure that empathy and humanism remain central to modern medicine, while increasing patient trust.
To accomplish this, we need better medical education and policymaking. Medical schools must go beyond hard sciences and clinical teaching to educate future physicians on emerging technologies that may play a role in their daily practice. This can ensure appropriate use and allow physicians to guide the basic design of these technologies and keep patients’ needs at the forefront.
Similarly, health policymakers must ensure this technology is incorporated in a productive and safe manner. AI must not exacerbate inequity, as studies have shown concerns in this space. We must also limit unsupervised use of the technology in experimental ways without appropriate controls. Much like the process for approving new drugs, we should validate these technologies before widespread introduction.
By establishing national guidance and infrastructure on appropriate use, we can ensure that hospitals are using AI to help patients while maintaining trust in the system.
Yash B. Shah is a fourth-year medical student at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Please enable JavaScript to view the