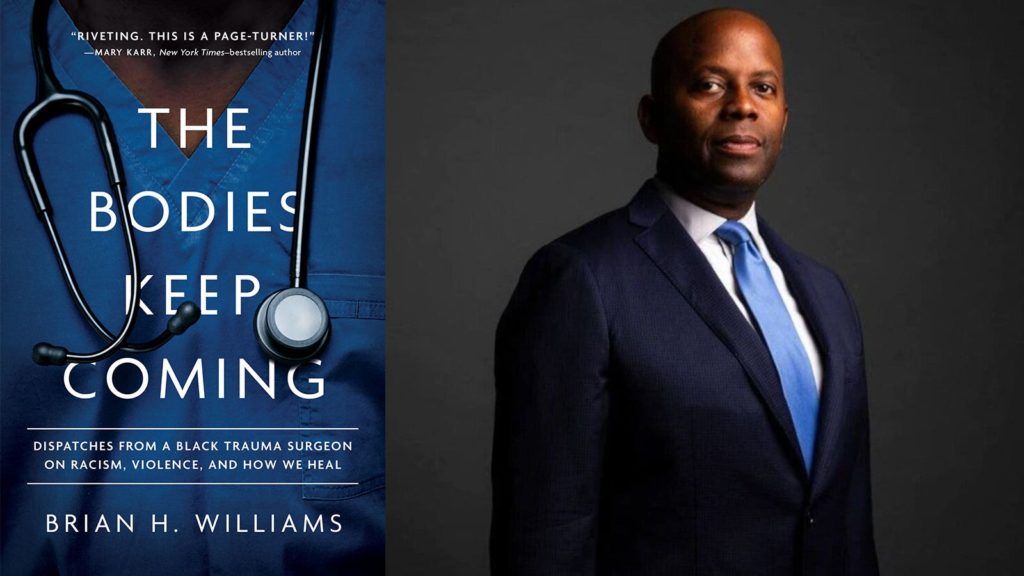
Brian H. Williams, MD, is a trauma surgeon.
Grady Memorial Hospital in Atlanta, Georgia, first opened as a 14-bed public hospital in 1892, the same year the first immigrants passed through Ellis Island. Grady Hospital is also where I trained to become a trauma surgeon and critical care specialist. It’s hard to imagine a clearer manifestation of the racialized U.S. healthcare system than Grady Hospital. During the Jim Crow era, Atlantans referred to the hospital in the plural form — “The Gradys” — because it was essentially two different hospitals contained in a single building. During my fellowship training, many of the elders I cared for still referred to it as such. For many years, Grady had four wings: A and B wings for white patients, with enviable views of the city, and D and E wings on the opposite side for Black patients, with views of neighborhood blight. A long hallway connected the two segregated wards, and Black doctors were disallowed into the hospital to care for their own patients who had been admitted.
As the years progressed, I took for granted how much care patients received without oversight by more senior doctors. Day-to-day decisions at Grady were relegated to fellows, residents, and interns. We can debate whether this was a superb learning environment for surgical trainees or medical exploitation. What is beyond debate is that when the same trainees cared for patients across town at the university hospital — which mostly served wealthy, white patients — they had more stringent oversight.
A roiling history of exploitation of and experimentation on Black people has fostered distrust of the medical establishment. A brief survey of history includes J. Marion Sims, MD, past president of the American Medical Association and often revered as the “father of modern gynecology,” who performed barbaric vaginal operations on enslaved women. They were denied anesthesia, physically restrained, and repeatedly mutilated. Involuntary hysterectomies — what Fannie Lou Hamer came to call the “Mississippi appendectomy” — were frequently performed on Black women, often by medical students in training. These are part of the legacy of “dehumanizing attempts to control Black women’s reproductive lives,” as Dorothy E. Roberts describes in Killing the Black Body.
You are likely aware of the Tuskegee Syphilis Study: the multigenerational study run by the federal government, in which the U.S. Public Health Service denied 600 Black men therapeutic penicillin from 1932 to 1972 to allow the study of the natural progression of latent syphilis. You may not be aware that the Pentagon funded a study of non-therapeutic, whole-body irradiation from 1960 to 1971. All the subjects were poor, most were Black, and 25% of the subjects died within 1 month of exposure. The Radiological Society of North America awarded the lead researcher-physician its highest honor. They conducted this research through the 1960s, as the U.S. prepared to land men on the moon, and the study did not end until the year before my younger sister was born.
Harriet Washington documents these studies and more in Medical Apartheid. And as Washington demonstrates in Carte Blanche: The Erosion of Medical Consent, academic medical centers, like the ones where I have spent my entire career, were placed geographically precisely to exploit this reality. But Washington says it best: “Many medical institutions are located in predominately African-American and poverty-stricken areas…This is not accidental but by design. The proximity of Black bodies for display, teaching, practice, and training material was an economic boon for medical schools and a selling point in recruiting medical students.” To be clear, academic medical institutions were collocated, by design, adjacent to racially segregated, poverty-stricken neighborhoods. What better way to recruit medical trainees than to boast of the amazing opportunities to hone their craft? Where better to literally “practice” medicine than in a community of de facto experimental subjects who have no other options?
When I came of age in the 1980s, Black women, many of them in their teens like me, were still the prime target for controlled reproduction through forced sterilization. And in the 1990s, the Medical University of South Carolina enrolled pregnant Black women in drug addiction research without their knowledge. Take a critical look at your nearest academic medical center, and you are likely to find the exploitation still thriving.
Even today, Black Americans, identified with euphemisms like “urban poor” or “socioeconomically disadvantaged,” still serve as a ready supply for medical research. The era of involuntary experimentation has evolved into a complex system of “waiver of consent,” used as a procedural means to circumvent obtaining informed consent. From 1996 to 2017, 46,964 patients were enrolled in 41 trials for modern therapeutic drugs and medical devices, in which the FDA granted an “exception from informed consent,” or EFIC. In EFIC trials, which are designed for patients with life-threatening conditions, subjects are required to opt out, rather than opt in. That means that in certain situations, you can be enrolled in a study without your informed consent. Of the nearly 47,000 patients enrolled in these studies, 96% were enrolled without their consent. Many interventions had adverse effects, including death. And nearly one-third of the research subjects were Black Americans.
You can make cogent arguments that this work is legal and necessary to advance medical science. But legal does not mean ethical. Ethics and equity demand a higher standard, and research requires relationships, not paternalism. It requires respect, not exploitation. When I started medical school, I had no idea my life as an academic surgeon would make me complicit in a system built on the invisible exploitation of the bodies of my people. We practice medicine on vulnerable Black people. We perfect our surgical techniques on broken Black bodies.
During my years at Grady, my laser-focus was to become one of the top trauma surgeons on the planet. I did not believe I could do anything more than perfect my skills, save lives one at a time, and teach others what I knew. These were nothing more than bullet wounds to me; as a trauma surgeon, I could repair the wound. But to question what kept the bodies coming to my trauma bay in the first place? To repair the upstream societal ills that funneled the bodies toward the hospital? I didn’t even think to ask. I kept my head down and scalpel ready for the next trauma.
Brian H. Williams, MD, is a trauma surgeon in Dallas and a candidate for U.S. Congress. He is also a member of the MedPage Today editorial board. This excerpt has been reprinted with permission from Williams’ forthcoming book, The Bodies Keep Coming: Dispatches from a Black Trauma Surgeon on Racism, Violence, and How We Heal, copyright © 2023 Broadleaf Books.
Please enable JavaScript to view the