Muth is a primary care pediatrician and obesity medicine specialist.
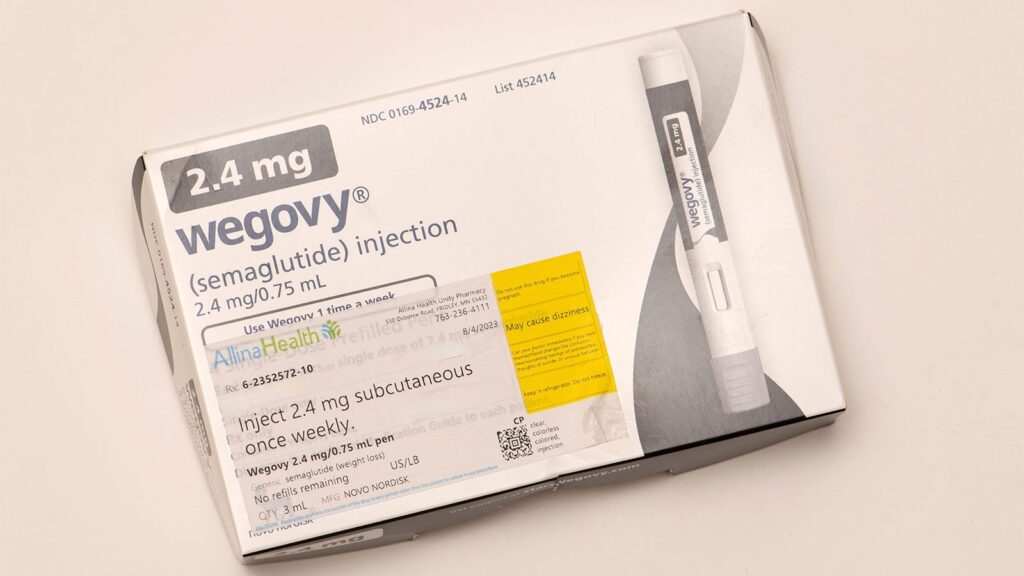
As a pediatric obesity medicine specialist, I have witnessed first-hand the benefits of GLP-1 receptor agonists in the treatment of adolescent obesity. In particular, semaglutide (Wegovy) plus intensive health behavior lifestyle treatment has improved comorbid health risk factors, physical activity tolerance, sleep, body image, and self-confidence in many of the adolescents that I care for at a primary care-based clinic.
But for the many younger children (under 12 years old) I see, no matter how severe the obesity or significant the obesity-related risk factors — like prediabetes, fatty liver, hypercholesterolemia, sleep apnea, or bullying and psychosocial distress — no medication options are approved to accompany intensive health behavior lifestyle intervention.
That may all change soon.
The FDA is currently considering approval of liraglutide for the treatment of severe obesity in children ages 6-12. The review comes on the heels of a randomized trial published in the New England Journal of Medicine (NEJM) demonstrating the safety and efficacy of liraglutide, added to lifestyle intervention, in treating severe obesity in this patient population.
Specifically, the multicenter trial of 82 kids found that over a 56-week treatment period, children treated with 3 mg of liraglutide plus behavioral intervention experienced a 5.8% decrease in BMI compared with a 1.6% increase in the behavioral intervention only group. Of those children who received liraglutide, 80% experienced gastrointestinal side effects, most of which were mild or moderate, compared to 54% in the placebo group.
Although the American Academy of Pediatrics’ Clinical Practice Guideline says we “may offer children ages 8 through 11 years of age with obesity weight loss pharmacotherapy, according to medication indications, risks, and benefits, as an adjunct to health behavior and lifestyle treatment,” FDA approval is a necessary step before I will prescribe obesity medications in children younger than 12 years.
But still, FDA approval is not a game-changer for me. As I consider the risks versus benefits of liraglutide in this population, I anticipate benefits outweighing risks in only a select few situations. Here’s an overview of what I see as the risks and benefits:
Benefits:
- Modest reduction in BMI percentile during the treatment period.
- Possible improvements in metabolic risk factors. (Although the trial did not find statistically significant improvements in blood pressure or hemoglobin A1c, there were trends toward improvement.)
- Possible improvements in psychosocial risk factors associated with severe obesity (based on findings from studies of adolescents taking obesity medications), but this was not studied in the trial of liraglutide in kids 6-12.
Risks:
- Unknown long-term safety and efficacy, including impact on growth and adult height.
- Side effects, including unknown long-term side effects.
- Weight gain once medication use stops. In this trial, children in the treatment group gained back nearly all the weight lost after 26 weeks off of the medication (at 82 weeks, the weight was -0.8% in the treatment group compared to +6.7% in placebo group). An open-label extension phase of the trial is ongoing, which will better elucidate longer-term outcomes.
- Daily injection required.
Severe obesity is a disease that requires individualized treatment. In some cases, this may include GLP-1 medications for children ages 6-12 if they are FDA-approved, and following close consideration and discussion of risks, benefits, and unknowns with caregivers, and only alongside an intensive health behavior lifestyle intervention. For me, the risks outweigh the benefits of pharmacological treatment of severe obesity in children ages 6-12 most of the time.
However, if FDA approves liraglutide for children, having it as a treatment option is meaningful. My risk-benefit analysis may change as more medication options and longer-term studies of safety and efficacy become available. I am grateful to the researchers studying these treatments in children, ensuring that kids are not left behind in the obesity treatment revolution, but we must proceed with caution.
Natalie Muth, MD, MPH, MBA, RDN, is a primary care pediatrician and obesity medicine specialist in the WELL Clinic at Children’s Primary Care Medical Group in Carlsbad, California, and co-founder of Namio Health, a virtual intensive behavioral intervention for the treatment of pediatric obesity.
Please enable JavaScript to view the