Sekeres is a leukemia specialist.
My patient was young, in his thirties, and had a terrible leukemia that refused to be vanquished with multiple rounds of chemotherapy. Many of my adult patients, at the time of their diagnosis, tell me they are so happy they have acute lymphoblastic leukemia, and not acute myeloid leukemia, because “that’s the good one — the leukemia that kids get.” Good when it goes quickly into remission and stays there, awful when it doesn’t.
And my patient’s leukemia didn’t stay in remission. We had reached that difficult point in our discussion about treatment when we adjust our goals. Now, rather than cure, we hoped that chemotherapy or monoclonal antibodies could eradicate the leukemia just long enough to get him to the cellular-based approaches — either hematopoietic cell transplantation or one of the newer CAR T-cell therapies — that might give him a better shot at a lengthier survival.
With the recent news of the FDA adding black box warnings to the labeling of all approved CAR T-cell therapies, given the risk for secondary T-cell malignancies, it naturally begged the question of whether this should remain a viable treatment option for any of my patients.
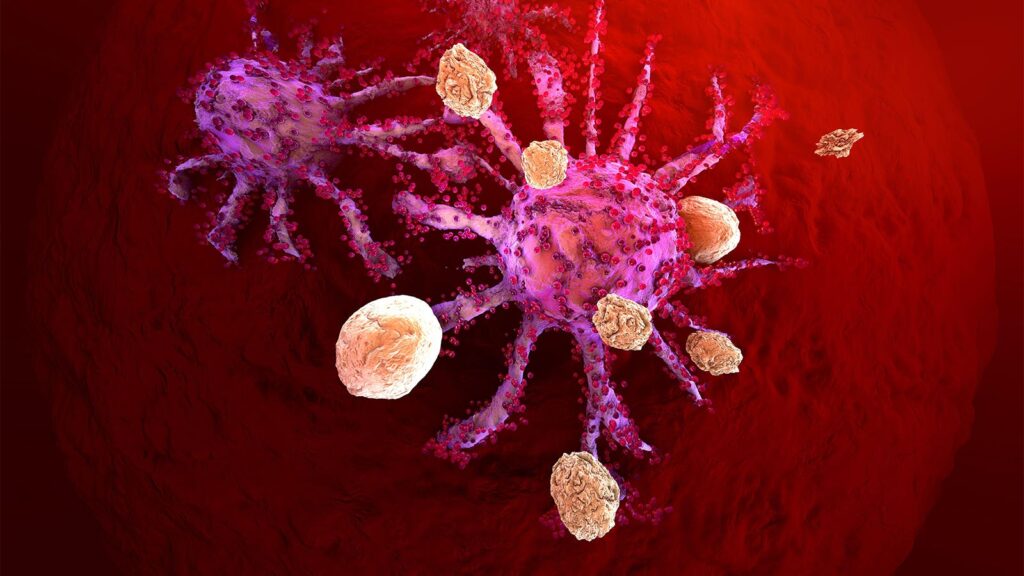
CAR T-cell approaches are the stuff of science fiction: We filter a patient’s blood to get a sample of their immune system, re-engineer it to have a monomaniacal focus on killing that patient’s own cancer cells, and re-infuse the mixture as we watch the patient’s cancer recede — and it works most of the time! At least for a while. Is it any surprise though, as we monkey around with the immune system, that cancers of the immune system such as lymphoma might arise?
Probably not. Perhaps the real surprise should be that it happens so infrequently.
The FDA has identified at least 22 patients who developed secondary T-cell malignancies so far, out of tens of thousands of people treated with CAR T-cell approaches. That’s a risk ratio of approximately 1 in 1,000 in patients who, by the way, had also received traditional chemotherapy prior to the CAR T-cells — chemotherapy that itself can damage cells enough to cause secondary malignancies. I should know — for years I have seen patients in my own clinic with secondary myelodysplastic syndromes or leukemias following similar chemotherapy. Compare that 1 in 1,000 risk to the high risk of the recalcitrant leukemia, or lymphoma, or multiple myeloma marching on (if active), or returning with a vengeance if a patient is in remission.
Should our patients be worried about the new black box warnings? Risk of acquiring another cancer is not small potatoes.
There is the larger question, however, of whether black box warnings are actually effective. Critics of the label point out that physicians are not very compliant with the warnings, with one study showing that physicians adhered to the warnings less than 50% of the time. Additionally, black boxes may discourage some patients from taking their medications. Colleagues of mine have already told me stories of patients who are now reluctant to consider CAR T-cell treatment in light of the news about secondary T-cell lymphomas. Finally, the FDA has been called out for a lack of transparency regarding the criteria it uses to issue a black box warning requirement.
I don’t think our patients should be concerned about CAR T-cells any more than they would be about other cancer therapies. When we offer treatments for cancer, unfortunately there are no free rides — every effective cancer therapy has the potential to cause side effects, and we are willing to accept some pretty major side effects when we are treating life-threatening diseases. If I were told that I could receive a treatment for relapsed cancer that had an 80-90% chance of working, with a 1 in 1,000 risk of getting another cancer, I would definitely decide to take the therapy and accept that risk. That’s what my patient decided, too.
What about doctors? Should we worry about the new FDA warning? I will still recommend CART-cell therapies for my patients as I always have, and will incorporate a discussion of the risk of another cancer, just as I do with other cancer treatments. The potential benefit of the therapy still far outweighs the risk of another cancer.
In fact, I applaud the FDA for including the additional risk in the safety labeling for CAR T-cell therapy so all of us — physicians and patients alike — go into a treatment approach with eyes wide open.
Mikkael A. Sekeres, MD, MS, is chief of the Division of Hematology and professor of medicine at the Sylvester Comprehensive Cancer Center at the University of Miami. He is author of the books, When Blood Breaks Down: Life Lessons from Leukemia (The MIT Press 2020), and Drugs and the FDA: Safety, Efficacy, and the Public’s Trust (The MIT Press 2022).
Please enable JavaScript to view the