Diabetes and obesity GLP-1 drugs like Ozempic, which can delay stomach emptying, have introduced a predicament for patients undergoing surgeries and endoscopies — the patients in some cases may still have food in their stomach even if they’ve fasted, raising concerns that they could accidentally breathe food into their lungs during the procedures.
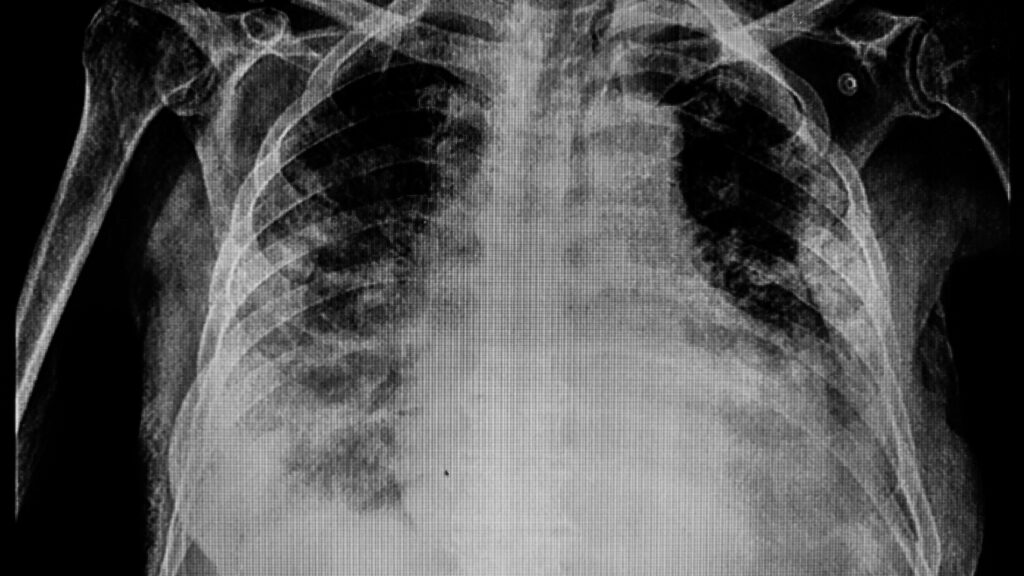
These concerns have been based on anecdotes, and it’s so far unclear how big an issue this is, but a new study published in Gastroenterology Wednesday offers some early clues. It links GLP-1 drugs to a higher risk of aspiration pneumonia — lung infection caused by food breathed into the lungs — following endoscopies.
advertisement
Researchers, analyzing a large dataset of health records, found that people taking GLP-1 drugs overall had a very low 0.83% risk of this infection, but they had a 33% greater risk compared with people who weren’t on GLP-1 treatments.
Zooming in on the different types of endoscopies, the researchers found that among people undergoing upper endoscopies, GLP-1 drug users had an 48% higher risk of aspiration pneumonia, and for combined upper endoscopies and colonoscopies, they had more than double the risk. The researchers did not find a higher risk among people getting only colonoscopies.
For patients who used the sedative propofol for their endoscopies, GLP-1 users had a 49% higher risk of aspiration pneumonia, according to the analysis, which included records of nearly 800,000 patients.
advertisement
The study looked at data from 2018 to 2020, when Ozempic had already been on the market, but before the latest GLP-1 treatments like Wegovy, Mounjaro, and Zepbound were approved. It’s unclear how exactly these newer and more potent treatments might affect patients’ risk for aspiration, but they do utilize the same or similar drug mechanisms as Ozempic, and the study points to the need for more research to help guide doctors as more people start taking these highly popular medications.
“They’re here to stay and their use is going to increase. They just have this complication,” said Ali Rezaie, senior author of the study and medical director of the GI Motility Program at Cedars-Sinai. “This is all about awareness. This is not about, ‘OK, let’s not use GLP-1s’ or anything. It’s just about, ‘let’s be careful when you’re doing procedures on these patients.’”
Prior to this study, two doctor groups issued differing statements about what to do with GLP-1 drugs before procedures. The American Society of Anesthesiologists suggested that patients should stop taking the treatments ahead of procedures. Meanwhile, the American Gastroenterological Association said that there is insufficient evidence for a formal guideline and suggested doctors should evaluate each patient individually.
Barbara Jung, president of the AGA, said that given the limitations of the study, she doesn’t think it would change what the association said in its statement, and “we need more information before we would.”
This study is limited as it’s observational and does not prove that GLP-1 drug use causes an increased risk of aspiration. Despite the study’s reliance on health records, the researchers could not confirm how consistently patients were taking GLP-1 drugs before the procedures. Also, they included cases of aspiration pneumonia that occurred within a month of the procedures, but had no way of confirming whether the infection necessarily stemmed from the procedures.
Rezaie, the senior author, said that even though the absolute risk of aspiration pneumonia for people taking GLP-1 drugs was under 1%, there are more than 20 million endoscopies performed in the U.S. each year, so a small percentage could amount to many cases. And while aspiration pneumonia can often be treated with antibiotics, they can cause complications in some cases for people who are immunocompromised or have pre-existing lung problems, he added.
It’s likely there is a higher risk in procedures that involve upper endoscopies specifically, since the patient is intermittently lying down and their stomachs get expanded with carbon dioxide, which can increase the chances of aspiration, the authors wrote. There is probably also a higher risk with the use of propofol, since the sedative blocks the body’s reflexes for protecting the airway, the authors said.
They note that not all cases of aspiration during endoscopies result in aspiration pneumonia, and so there were likely many more cases of aspiration that weren’t captured in the study.
Given the study design, the study should be considered “as mainly hypothesis-generating,” said Andrew Wang, chief of the division of gastroenterology and hepatology at University of Virginia who was not involved in the study. Wang co-authored the AGA statement about the use of GLP-1 drugs.
He noted that the study also doesn’t provide information on whether stopping the drugs ahead of procedures would mitigate the risk of aspiration.
Overall, though, he said, “this study is important as we need more data about the possible consequences for patients using [GLP-1 drugs] prior to GI endoscopy.”
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.