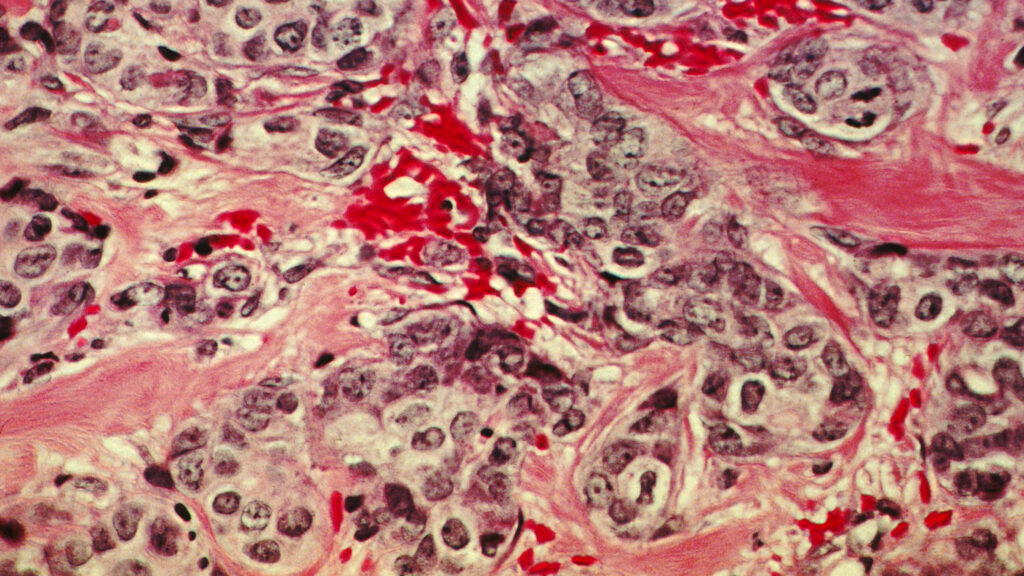
Early-stage cancer diagnoses decreased by nearly 20% in the first year of the Covid-19 pandemic. A new study published in Lancet Oncology emphasizes how, because of disruptions in care, patients were more likely to get diagnosed with deadly metastatic disease — across nearly all cancer types.
This study is the most comprehensive analysis of cancer diagnoses during the pandemic, using a nationwide registry that captures over 70% of all cancers in the United States. The starkest decline was observed after the initial shutdowns, with the regular 70,000 monthly cancer diagnoses (captured by the study’s inclusion criteria) being cut in half in April 2020.
advertisement
While some cancers can be detected by screening — such as lung, breast, colon, and cervical — others require access to primary care, timely referral to specialists, and diagnostic tests. In the early months of the pandemic, however, much of this went silent, according to Hannah Hazard-Jenkins, director of the West Virginia University Cancer Institute, who was not involved with this study. “We ended up shutting down everything that was ‘elective’ in anticipation of a large volume of patients with Covid.”
Hazard-Jenkins described how WVU began to reopen in June 2020. But that didn’t mean patients were comfortable enough to return. “Which is worse: dealing with the potential of getting Covid-19 with such a high fatality rate versus dealing with a concern for a cancer diagnosis?” asked Hazard-Jenkins. “That was a real struggle for patients.”
Xuesong Han, the lead author of this study and scientific director of health services research at the American Cancer Society, said that monthly cancer diagnoses returned to a “near pre-pandemic level” in June 2020, hovering at around 60,000 monthly cases for the remainder of the year. “Has it returned to pre-pandemic level now?” she asked. “We cannot tell as the data are not available yet.”
advertisement
What Han’s data did clearly show is that stage 4 cancer diagnoses were 7% more likely in 2020 and that communities of color were particularly hard hit, suggesting significant long-term consequences. Indeed, with nearly 2 million new cancer diagnoses each year, these diagnostic delays could lead to tens of thousands of additional patient deaths and tens of millions of dollars in added health care costs.
Lung cancer, for instance, is responsible for about 1 in 5 of all U.S. cancer deaths, killing more people than breast, colon, and prostate cancer combined. If caught in its early stages, the five-year survival rate is 56%; in its late stages, that number drops to just 5%. Similarly, while stage 1 lung cancer costs a median $25,000 to treat, stage 4 lung cancer costs almost ten times as much at $210,000.
As a breast cancer surgeon, Hazard-Jenkins described seeing patients in late 2020, who knew they had a lump since April but “didn’t do anything because of their fear.” What would have normally been treated by a simple lumpectomy “had to be forced into mastectomy.” Patients who would otherwise receive curative treatment were now getting palliative care because their tumors had metastasized beyond relief.
And these trends have been continuing beyond 2020. “In the breast cancer world, last year we had a profound amount of advanced disease,” said Hazard-Jenkins. “It was numbers of advanced disease I haven’t seen in 15-plus years.”
The study found that marginalized populations were particularly impacted by these late-stage cancers, with Hispanic Americans and Asian Americans and Pacific Islanders being 10%-11% more likely to receive a stage 4 diagnosis in 2020.
Han explained that these racial and ethnic disparities could possibly be explained by cultural and language barriers, low trust in the health care system, and financial shocks due to losing employment. But she particularly emphasized that racial discrimination intensified during the pandemic and could potentially explain why these groups delayed or skipped care. Indeed, during the first year of the pandemic, 1 in 6 Hispanic individuals and 1 in 5 East and Southeast Asian Americans reported facing racial discrimination.
Patients living in socioeconomically deprived areas, largely represented by rural, Indigenous, and historically redlined communities, were similarly 11% more likely to receive a stage 4 cancer diagnosis. “When you’re talking about low health literacy coupled with low financial resources coupled with geographic challenges, it can be very difficult to seek health care,” said Hazard-Jenkins.
Both Han and Hazard-Jenkins thus underscored that, to address these disparities and the impact of delayed cancer diagnoses, the health care system should do a better job of meeting people where they are. “Efforts can be made to continue some silver linings from the pandemic,” said Han, such as “wide adoption of telemedicine and increased use of home-based stool testing for colorectal cancer screening.”
Hazard-Jenkins also described mobile screening programs as another way to engage underserved communities. Since 2009, WVU has been running Bonnie’s Bus for early breast cancer detection and, since 2021, the LUCAS tractor-trailer for lung cancer, with both units driving to the most rural communities in West Virginia to get patients screened. With decade-long partnerships with local providers and federally qualified health centers, Bonnie’s Bus and LUCAS screened a combined 3,750 patients across the state in 2022, regardless of their ability to pay. “When you have economically challenged communities, socially challenged communities and us as big health systems, having this expectation of people coming to you is really just naive,” said Hazard-Jenkins.
It takes similarly creative strategies to ameliorate racial and ethnic disparities, said Priti Bandi, a scientific director at the American Cancer Society. She noted that, while evidence is generally limited, community-based interventions have previously helped improve screening rates among Asian Americans and Pacific Islanders and Hispanic Americans, with lay health workers educating patients in their homes, churches, and grocery stores.
Beyond addressing disparities through greater awareness, the health care system must focus on transportation issues, child care needs, and helping patients navigate through a complex health care system, according to Anne Hubbard, who is the director of health policy at American Society for Radiation Oncology and was not involved in this study. While the health care system doesn’t currently value these wraparound services, she said there are promising trends, such as the Centers for Medicare and Medicaid Services proposing payment for social determinants of health in the latest version of the physician fee schedule.
Absent these and other reforms to increase access to care, “we’re going to continue to see disproportionate numbers of disadvantaged patient populations who are presenting with more advanced stage disease,” said Hubbard.
Ultimately, Han is optimistic that, with return-to-screening campaigns getting the word out and routine doctor visits going back to normal, patients will increasingly have their cancers caught early and have better outcomes. But she also emphasized that challenges remain, such as nearly 4 million losing Medicaid insurance since pandemic-era protections expired in March.
“Disparities in care access and health outcomes have not been specific to cancer,” Han said. “Improving broader socioeconomic infrastructure for medically underserved communities is required.”