The incidence of Creutzfeldt-Jakob disease (CJD), a universally fatal prion disease that progresses rapidly, rose consistently from 2007 to 2020, a study of death certificates showed.
CJD codes on death certificates totaled 5,882 during that period, with 51.2% of cases occurring among women, according to John Probasco, MD, and Matthew Crane, BS, both of Johns Hopkins School of Medicine in Baltimore, and co-authors.
From 2007 to 2020, the incidence climbed from 1.06 to 1.58 per million in women (P<0.001) and from 1.05 to 1.47 per million in men (P=0.001).
After adjusting for age, the increase in incidence was not significant for men (P=0.25) but remained significant for women (P=0.045), Probasco and colleagues reported in a JAMA Neurology research letter.
“Our findings indicate the reported incidence of CJD has risen considerably, disproportionately affecting older and female individuals,” the researchers observed.
CJD is the most common form of human prion disease. Approximately 85% of cases are sporadic and 15% are genetic. About 70% of people with CJD die within 1 year.
CJD presents as a rapidly progressing dementia and tends to strike people 60 and older. Variant CJD, an infectious type linked to bovine spongiform encephalopathy or “mad cow” disease, was first detected in the U.K. in the mid-1990s and usually affects younger people. Four cases of variant CJD have been reported in the U.S. since 2001. Other animal prion diseases like chronic wasting disease may have the potential for zoonotic transmission to humans, but no human cases have been reported.
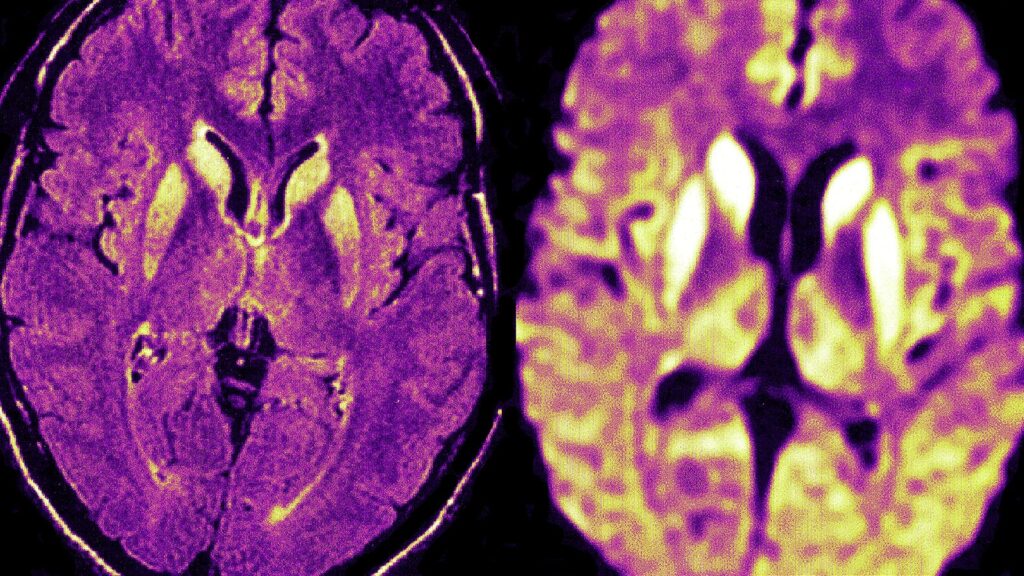
Diagnosing CJD has evolved over the years and now includes specific MRI characteristics and real-time quaking-induced conversion (RT-QuIC) tests to detect abnormally folded prion proteins. MRI diagnostic criteria were published in 2009 and RT-QuIC testing was introduced in 2015.
Probasco and colleagues evaluated information from the CDC WONDER multiple cause of death database and found CJD codes on 317 death certificates in 2007 and 502 death certificates in 2020.
Crude incidence showed a significant increase, with an average annual percent change of 2.9 for males and 3.5 for females. This fell to 0.8 for men and 1.9 for women after adjusting for age but was still significant. Men ages 55-64 were the only male age group with a significant increase. Women showed a significant increase in all age groups from 55-84.
The trends echoed recent findings from Japan and may be due to changing demographics, but could also reflect better CJD detection with new diagnostic tools like MRI and RT-QuIC testing, the researchers noted.
Because the study was limited by its reliance on death certificate data, miscoding or misdiagnosis may have occurred, Probasco and co-authors acknowledged. Nonetheless, “the findings underscore the changing landscape of CJD and suggest a need for monitoring among the aging U.S. population,” they wrote.
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
The researchers reported no conflicts of interest.
Primary Source
JAMA Neurology
Source Reference: Crane MA, et al “Change in epidemiology of Creutzfeldt-Jakob disease in the U.S., 2007-2020” JAMA Neurol 2023; DOI: 10.1001/jamaneurol.2023.4678.
Please enable JavaScript to view the