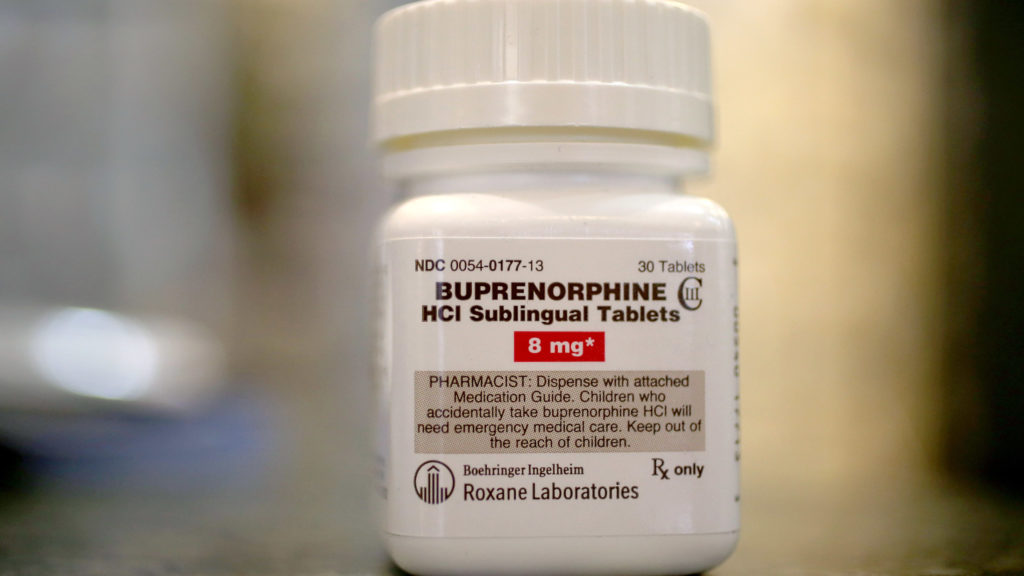
In December 2022, Congress repealed the “X-waiver” requirement, which had limited medical providers’ ability to prescribe buprenorphine-naloxone, one of the three medications approved by the Food and Drug Administration for the treatment of opioid use disorder. Lawmakers knew that the waiver was a major barrier to providing lifesaving medication that halves the risk of overdose to the millions of Americans needing treatment for opioid use disorder.
Yet, even with the waiver nixed and increasing recognition of the importance of access to treatment, the number of providers prescribing buprenorphine has not grown significantly. One analysis using emergency department data found that the percentage of encounters with patients with opioid use disorder that resulted in a buprenorphine prescription increased from 2% in 2019 to 8% in 2023. While this increase is encouraging, it is not the scale-up in treatment many hoped for.This raises a simple question: Why?
advertisement
It seems that providers simply don’t want to prescribe it more. As a public health researcher, I’ve heard critics express concern that more flexible prescription policies could lead to buprenorphine getting into the hands of someone without a prescription, also known as diversion.
But diversion is not something that they should fear so much. In contrast to diverting one of the prescription opioids that fueled the opioid crisis like oxycodone, sharing buprenorphine through informal channels could reduce the use of much more deadly opioids such as heroin and fentanyl. At least one study has shown that use of non-prescribed buprenorphine is protective.
To address this dilemma and evaluate the benefits and risks of non-prescribed buprenorphine, my colleagues and I at RTI International used a simulation model of people with opioid use disorder to estimate the impact of non-prescribed buprenorphine on overdose within a population. We found that increasing the amount of non-prescribed buprenorphine within communities decreased the number of overdoses by 3%-6%. This outcome might seem counterintuitive, but it is supported by data and matches my personal experiences as a public health professional.
advertisement
When I visited the streets of Kensington, Philadelphia, an epicenter of the opioid epidemic, in 2015, I often heard dealers shout, “Strips! We got strips!” referring to the sublingual (under the tongue) film formulation of buprenorphine-nalxone that is most commonly prescribed.
I was there to interview people who inject drugs for the National HIV Behavioral Health survey, overseen by the Centers for Disease Control and Prevention. At the time, I assumed these “strips” of buprenorphine were like oxycodone or the other prescription opioids being sold alongside bags of heroin. I thought they would further exacerbate addiction and pose a significant risk of overdose.
But I began to question my initial assumptions a few years later, after I completed my doctoral training in epidemiology at Brown University and began hearing from my husband, a physician at a federally qualified health center in Massachusetts who regularly prescribes buprenorphine to help patients manage their addiction.
He would tell me stories of patients who admitted to buying buprenorphine strips on the street to self-treat their addiction, allowing them to do things like travel out of town for a family member’s wedding or to bridge a gap in prescriptions. He had one patient who was not ready to stop using heroin or fentanyl but had taken non-prescribed buprenorphine for a weekend to be clear-headed for a job interview on Monday. After he started his job and received health insurance, he was able to begin formal buprenorphine treatment.
Research shows that sharing buprenorphine or selling part of one’s prescription is common. According to one study, up to half of individuals with a buprenorphine prescription will share or sell at least one strip from their prescription (a typical prescription is one to three strips per day) to help friends avoid using heroin or fentanyl or to prevent withdrawal. Most of this appears to occur informally — friends sharing a strip with someone who just ran out of their buprenorphine prescription or helping a friend who just lost their health insurance or job. In this way, non-prescribed buprenorphine could be considered a harm reduction measure, i.e., taking an action that lowers the risk of overdose.
In addition to an improved safety profile compared with other prescription opioids, research also suggests that people are unlikely to seek buprenorphine to get “high.” One study found that of buprenorphine poison exposures among young people 19 or younger, only 6% stemmed from seeking the euphoric effects of the drug. Structured analysis of internet forums like Reddit has found that people perceive buprenorphine strips as “weak.”
Due to its properties as a partial opioid agonist, buprenorphine is less likely to lead to overdose compared with full opioid agonists such as oxycodone. Of more than 27,000 buprenorphine exposures reported to the U.S. Poison Control Centers from 2003 to 2019, there were just 84 (0.3%) fatalities.
That does not mean it is harmless. Lessening restrictions does not obviate the need for patient education on safe storage practices to reduce the risk of accidental exposure for children. In addition, patients need to be aware that the risk of overdose rises significantly if using other substances including alcohol, stimulants, and benzodiazepines. Late actor Matthew Perry had therapeutic levels of buprenorphine in his system at time of death. While ketamine was determined to be the primary cause of death, patients should be counseled and aware of potential risks when combining buprenorphine with other substances or medications.
Liberalizing buprenorphine prescription policies will almost inevitably increase use of non-prescribed buprenorphine.
But the current evidence suggests that diversion is a form of harm reduction. We should continue making access to buprenorphine a low- to no-barrier proposition, and health care providers should set aside concerns about diversion and consider prescribing the medication to people who need it.
While not a panacea, recent policy changes, combined with a mindset shift, could go a long way to turning the tide on the opioid crisis that has claimed so many lives.
Joëlla W. Adams is an epidemiologist at RTI International, a nonprofit research institute. Her expertise includes simulation modeling and cost-effectiveness analyses, and she was lead author of the study that simulated the impacts of non-prescribed buprenorphine use.