A small study identified potential immunologic patterns associated with post-vaccination syndrome, a very rare condition with neurologic symptoms that occurs in some people following a COVID-19 vaccine.
Immune cell populations of people with post-vaccination syndrome had lower levels of effector CD4 T cells and higher levels of CD8 T cells that secrete tumor necrosis factor (TNF) compared with healthy controls, reported Akiko Iwasaki, PhD, of Yale University School of Medicine in New Haven, Connecticut, and co-authors in a preprint posted on medRxiv. The paper has not been peer-reviewed.
Post-vaccination syndrome patients had lower levels of antibodies against the SARS-CoV-2 spike protein versus healthy controls, likely because they stopped getting more vaccine doses, the researchers said. Evidence of recent Epstein-Barr virus (EBV) reactivation was seen more frequently in people with post-vaccination syndrome than in vaccinated people without the condition.
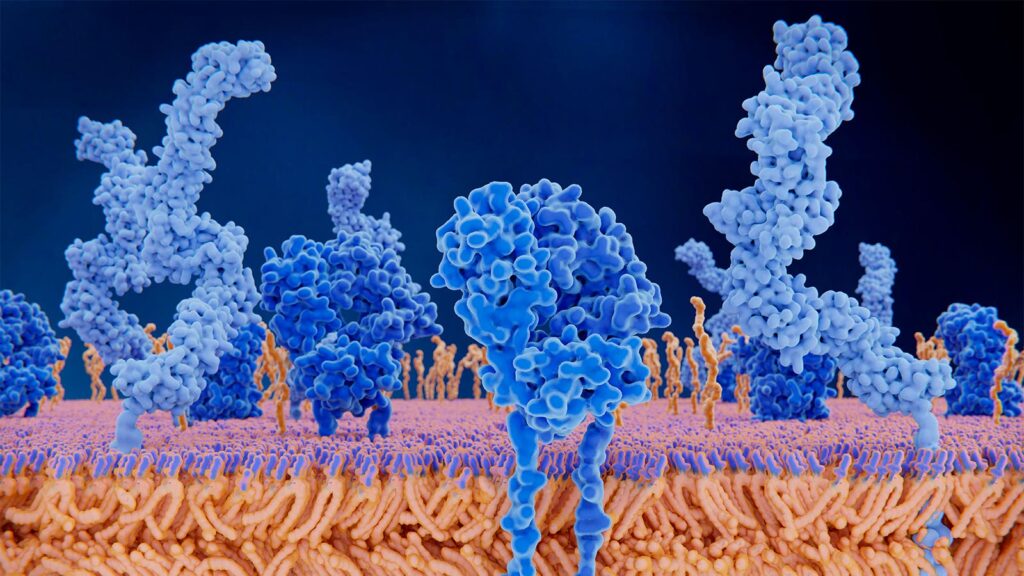
A subset of post-vaccination syndrome patients also had higher levels of circulating spike protein in their blood. Detectable levels of the S1 subunit of the spike protein were seen in plasma up to 709 days after the most recent known exposure.
Finding the spike protein in circulation at such a late time point was surprising, Iwasaki said.
“There is very little known about the biology of post-vaccination syndrome,” Iwasaki told MedPage Today. “We do not know how spike protein is present at such a long time from vaccination. We also do not know whether the spike protein is leading to illness in people.”
“Other studies have found that spike protein alone can induce fibrin clots and induce neuroinflammation,” she added. “We need to study this in larger patient groups and use multiple approaches to validate our findings.”
Persistent spike protein has been associated with long COVID, as has EBV reactivation. Like long COVID patients, people with post-vaccination syndrome often experience exercise intolerance or have persistent neurologic problems. A prior study reported that S1 spike expression on monocytes was elevated in people with post-vaccination syndrome who had long COVID-like symptoms.
“Post-vaccination syndrome and long COVID have many overlapping symptoms, but there are some distinct ones,” Iwasaki noted. “This possible overlap could be mediated by common pathological drivers such as spike protein or EBV reactivation.”
The immune findings came from an analysis of 42 people with post-vaccination syndrome (29 females and 13 males, all with no pre-existing comorbidities) and 22 controls who did not have post-vaccination syndrome after receiving a COVID vaccine (11 females and 11 males) from the LISTEN study. All blood samples were collected between December 2022 and November 2023.
The median age of participants was 42.5 years. The most frequent symptoms reported by those with post-vaccination syndrome were excessive fatigue (85%), tingling and numbness (80%), exercise intolerance (80%), brain fog (77.5%), difficulty concentrating or focusing (72.5%), trouble falling or staying asleep (70%), neuropathy (70%), muscle aches (70%), anxiety (65%), tinnitus (60%), and burning sensations (57.5%).
The study is limited by its small sample size and the fact that post-vaccination syndrome is “a very, very heterogeneous” disorder, noted Gregory Poland, MD, president of the Atria Health and Research Institute in New York City and emeritus editor-in-chief of the Vaccine journal.
“Despite these limitations, the researchers found interesting data that need further study, particularly in the arena of hyper-innate immune system activation and its consequences, persistent S1 protein circulating, and immune cell subset perturbations,” Poland told MedPage Today.
“My clinical impression is that post-vaccination syndrome is real,” he observed. “Collectively, my impression is that this adds to the growing body of literature and clinical experience suggesting that in rare cases, mRNA-based COVID vaccines can induce immune, autoimmune, viral reactivation, and other perturbations in susceptible individuals.”
Much larger studies of very carefully defined and phenotyped individuals are needed to be sure of that statement, Poland said. “But these investigators are approaching it correctly and pointing the way,” he noted. “After confirming these results, the next steps are to reverse-engineer vaccines to prevent this and to develop therapeutic approaches to reverse what has happened to these patients.”
-
Judy George covers neurology and neuroscience news for MedPage Today, writing about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more. Follow
Disclosures
This study was funded in part by the Howard Hughes Medical Institute Collaborative COVID-19 Initiative.
Iwasaki reported relationships with RIGImmune, Xanadu Bio, PanV, Roche Holding, and Genentech.
Co-authors reported relationships with government agencies and industry.
Poland reported that he has provided advice to every major vaccine manufacturer.
Primary Source
medRxiv
Source Reference: Bhattacharjee B, et al “Immunological and antigenic signatures associated with chronic illnesses after COVID-19 vaccination” medRxiv 2025; DOI: 10.1101/2025.02.18.25322379.
Please enable JavaScript to view the