If an effective treatment is available for one common disease in men, and that same treatment is available for a different common disease in women, a logical expectation would be that the treatments are equally accessible to men and women. That is not the current reality.
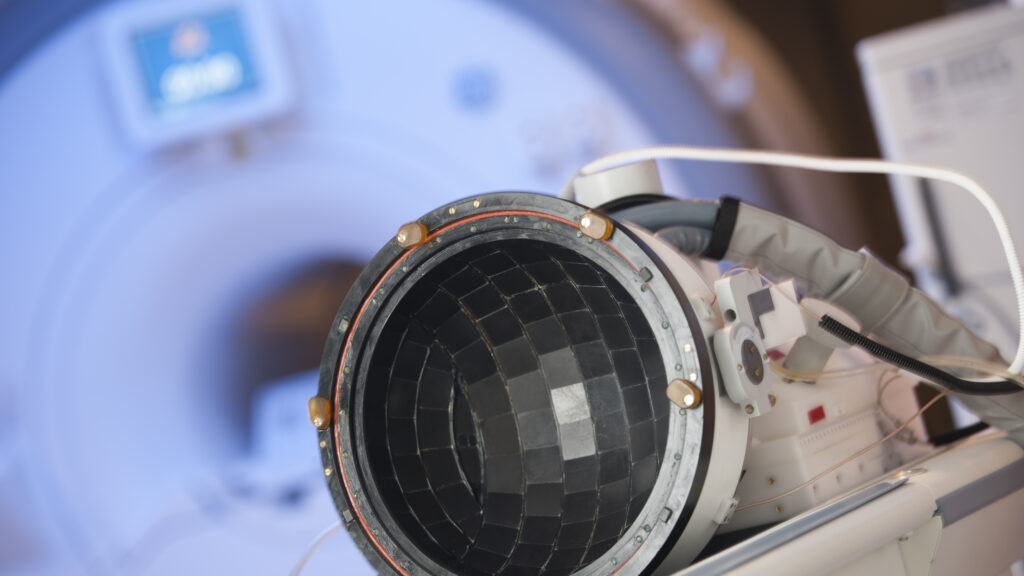
The treatment I am talking about is focused ultrasound. It has been approved by the Food and Drug Administration for a range of conditions, including prostate cancer, fibroids, liver tumors, essential tremor and Parkinson’s related tremor, osteoid osteoma, and pain from bone metastases. It works by using sound waves to precisely target and destroy tissue deep within the body without incisions or radiation. It’s akin to using a magnifying glass to converge the sun’s rays to a small spot on a leaf, causing enough heat to induce an actual flame. A focused ultrasound beam can be precisely focused on target tissue deep within the body to create heat to kill tissue, and the tissue in between is spared.
advertisement
For years, there were no good options for treating fibroids other than surgery, which many women were not interested in due to the risks, cost, and recovery time — not to mention the possible loss of their ability to have a baby if a hysterectomy was required. Minimally invasive procedures, utilizing catheters and probes that pierce through the skin or the cervix, exist such as uterine artery embolization and radiofrequency ablation, but they still carry risks and may require weeks of recovery. Medications can be helpful in temporarily shrinking fibroids and reducing some of the symptoms, but there are undesirable side effects associated with the decrease in hormone levels.
The FDA first approved focused ultrasound as a treatment of uterine fibroids in 2004. I had the privilege of performing the first commercial focused ultrasound treatment of uterine fibroids in the country. It was performed inside an MRI scanner; the patient was fully awake. She walked out of the medical center an hour after the procedure without any incisions and returned to her normal activities the next day.
Now, here is where the irony begins. Almost 300,000 men in the United States are diagnosed with prostate cancer each year; and millions live with enlarged prostate glands (benign prostatic hyperplasia), which can interfere with urination. They have access to more than 170 sites that offer focused ultrasound therapy, which is an FDA-approved treatment for both conditions. Medicare and most commercial insurers cover about 80% of the cost of this procedure.
advertisement
More than 25 million women in the U.S. live with uterine fibroids, growths in the uterus that can cause a range of debilitating symptoms, including excessive menstrual bleeding, severe pain in the pelvis and abdomen, and infertility. They have access to just seven sites offering FDA-approved focused ultrasound treatment, and only one private insurance carrier covers the procedure. The average out-of-pocket cost for treatment is around $40,000, making it inaccessible to most women.
A similar gap exists worldwide. Although more than 200,000 focused ultrasound treatments have been performed for fibroids and about 100,000 treatments for prostate disease, there are only 319 treatment sites for fibroids compared to 432 treatment sites for prostate cancer. One of the main reasons for this gap comes from the penalty of fibroids being the first indication approved, resulting in more scrutiny in the regulatory approval process, reimbursement approval process, and adoption by clinicians. There is more hesitation to adopt a disruptive technology that few clinicians were trained in. But it did pave the way for other clinical trials using focused ultrasound to move forward, leading to more indications approved by the FDA, reimbursed by insurance, and adopted by clinicians.
Additionally, there is a lack of representation among decision-makers who choose whether insurance pays for focused ultrasound for fibroids and how accessible it is. Few women are in leadership positions within focused ultrasound companies and insurance companies, and even fewer are African American women, who are more likely to have fibroids. This disparity is seen across health care, so much so that the White House recently announced a new initiative prioritizing women’s health research.
Twenty years after focused ultrasound was approved as a treatment for uterine fibroids, it is still the only noninvasive treatment for women with this condition. This technology has nine FDA-approved indications, yet this groundbreaking treatment remains hard to access for most women with fibroids in the U.S.
One of the most formidable challenges to making this therapy more accessible has been getting insurers to cover it, and thus few manufacturers are willing to enter the space. Despite extensive data demonstrating long-term efficacy and safety, insurance companies continue to dither by asking for additional evidence. Their reluctance is driven by cost concerns. Sixteen years ago I presented data showing the benefits of focused ultrasound for fibroids to insurers, but they believed treating a smaller subset of women with hysterectomy or even minimally invasive techniques is economically advantageous compared to offering focused ultrasound to the broader population of women with uterine fibroids.
The slow adoption of focused ultrasound for treating uterine fibroids isn’t for lack of women interested in the treatment. A survey published in the Journal of Women’s Health reported that when 1,000 U.S. women with fibroids were presented with descriptions of various treatments, 60% rated focused ultrasound as their top choice.
The U.S. health system is past due for change. Insurers must provide coverage for focused ultrasound as a treatment for uterine fibroids, and more manufacturers must enter the U.S. market, providing affordable systems for hospitals and clinics. It is imperative to seize this opportunity with the national spotlight on women’s health with the White House Initiative on Women’s Health Research to ensure that focused ultrasound becomes not just a promise but a reality for all women battling uterine fibroids.
Suzanne LeBlang, M.D., is a neuroradiologist who has performed hundreds of focused ultrasound procedures, the director of clinical relationships at the Focused Ultrasound Foundation, serves on the faculty at the University of Miami Miller School of Medicine, and is a clinical affiliate associate professor of medicine at the Florida Atlantic University Schmidt College of Medicine.